Podcasts Joelleen – midwife, IBCLC
EPISODE 450
Joelleen – midwife, IBCLC

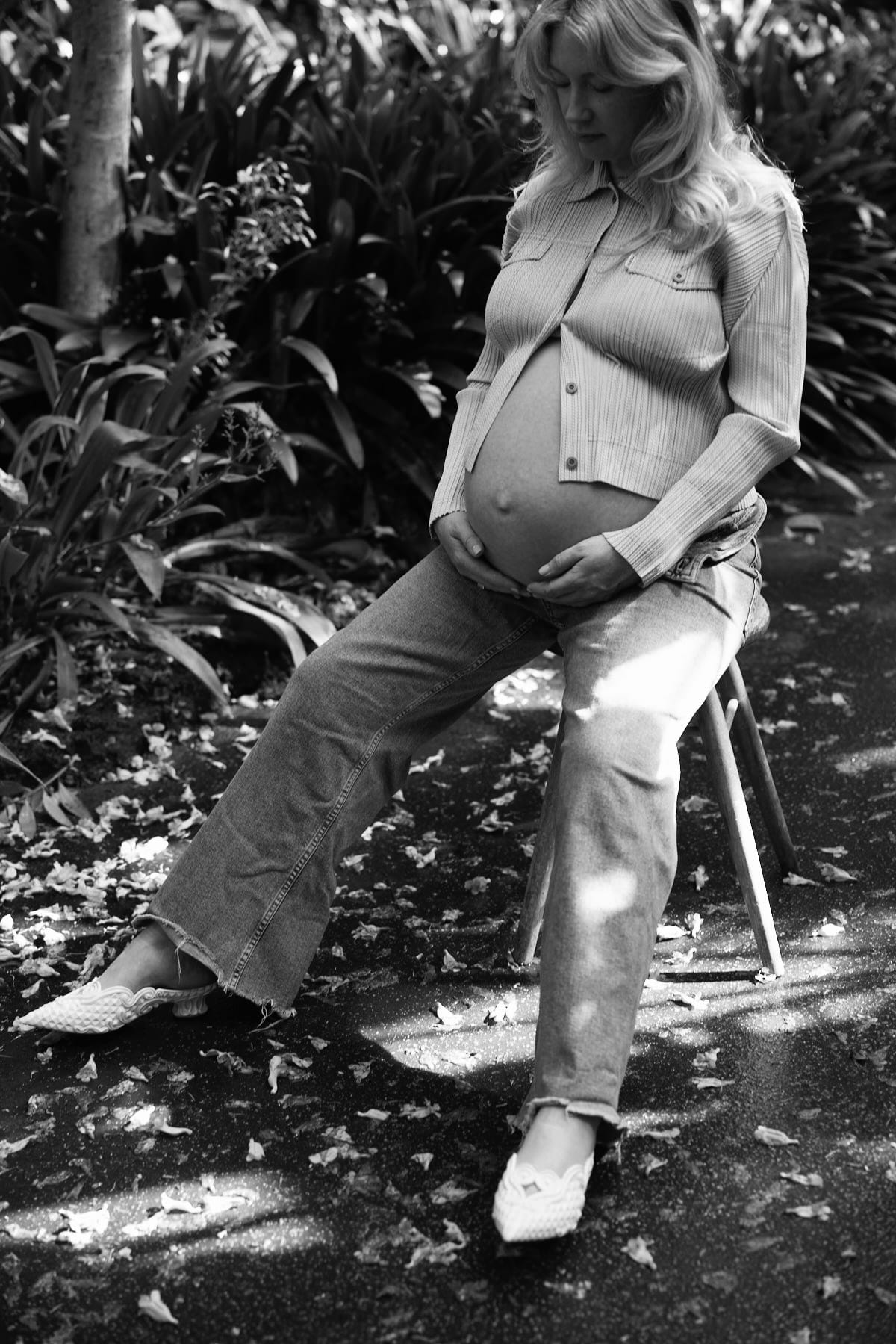
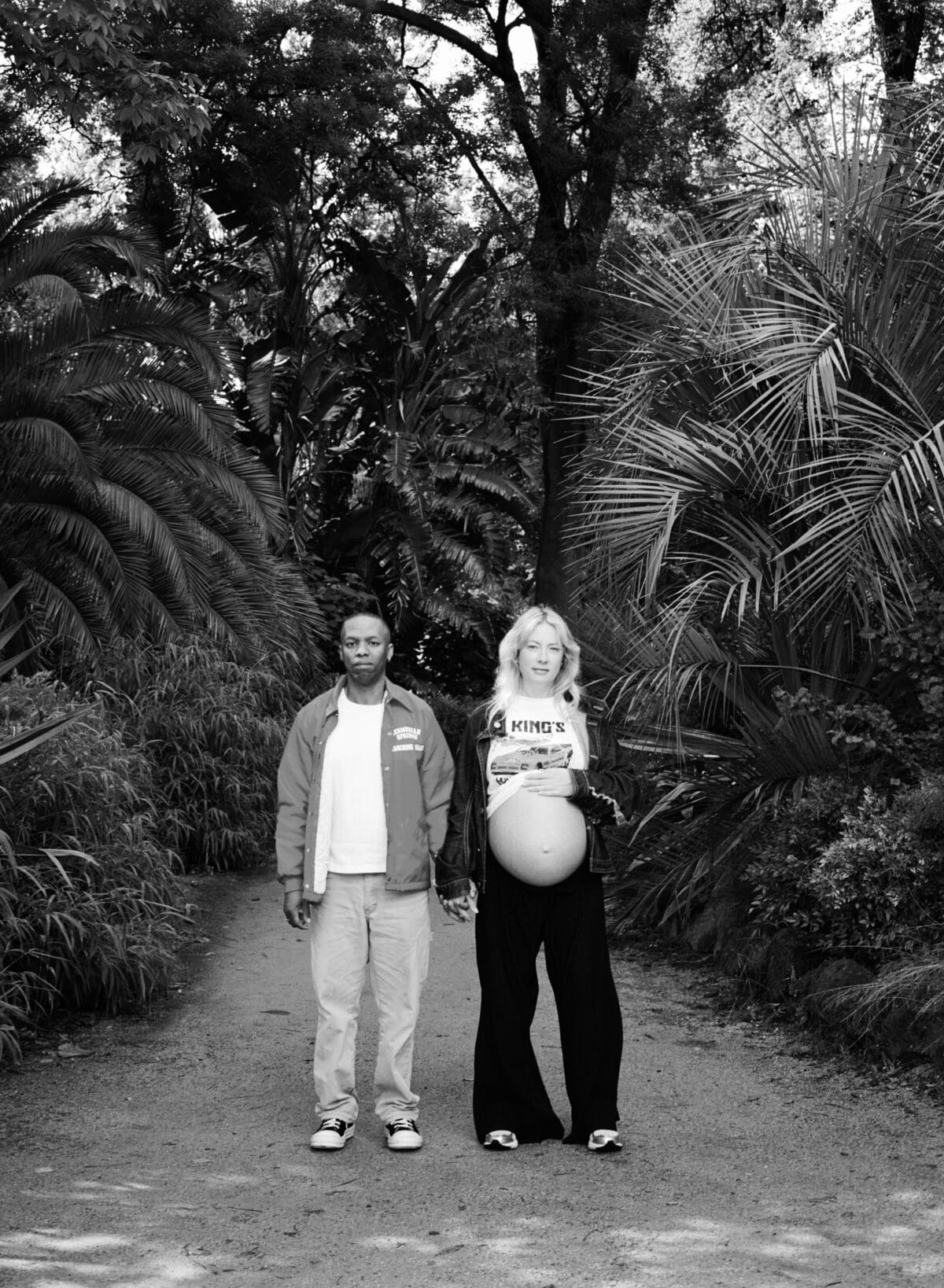
“In 2022 we decided to stop trying to avoid pregnancy and we conceived soon after. I was over the moon to be pregnant after so many years of supporting pregnant and postpartum mothers. At 13 weeks I had a bleed which was a subchorionic hematoma and it worried me, it was quite a lot of fresh blood and I thought I was going to miscarry. The pregnancy continued for another three weeks and then one night I went into spontaneous labour but I didn’t realise that’s what was happening. When my waters broke I knew nothing could be done so I stayed home and birthed my baby girl.
“That birthing experience really helped to inform my preparation for early labour with my second baby and I knew what I wanted and needed; privacy, darkness, peace and quiet. It was an early birth but it was quite physically demanding and I knew I had to trust my body. We just let nature take its course. One of the most physically and emotionally painful experiences was when my milk came in; I had such an abundant supply and breastfeeding is something I’d so looked forward to as a midwife and IBCLC. I was so grief-stricken that I wasn’t thinking of the biology of postpartum and I was so engorged. It was so heartbreaking having nowhere for all that milk to go. I used ice and took panadol and it settled. I didn’t want to touch my breasts because I knew expressing would prolong the fullness.
“The grief was very overwhelming and I felt so unprepared for postpartum. I tested positive to covid and in a way that really forced me to rest. We waited six months to start trying again because I didn’t feel like I was resilient enough to conceive and then lose another baby. There were days where all I wanted was to be pregnant and have another baby but I’m really glad we waited and preserved our emotional health.
“I really ummed and ahhed about what care model I wanted for my second pregnancy but I knew in my heart that I wanted a homebirth. It was an intuitive decision for me but I’m glad we took our time to figure out what felt right. We did some counselling around our birth choices, including an amazing session with Rhea Dempsey which really helped my husband understand birth and feel comfortable with our choice.
“I reached out to the Sunshine Hospital Homebirth programme and they assigned me to a midwife; I feel really blessed to have had a publicly-funded homebirth. I was on a foetal surveillance programme because of my previous loss but I never had concerns about an incompetent cervix.
“At 20 weeks I was more relaxed and excited and that’s when I publicly announced my pregnancy. I was so excited to start antenatal expressing and I was getting 1-3 ml a day. I’m so glad I did that because we had a short stint in NICU after birth and the colostrum was so beneficial.
“I knew if I went past 41+6 I wouldn’t be able to homebirth but thankfully I birthed at 40+4.On Christmas Eve I felt a bit crampy but nothing eventuated. Call me crazy but we were going to host a simple brunch but I didn’t feel like having people over so we went to my brother-in-law’s house and took a hot water bottle with me. After lunch I felt the need to be active, I needed to be moving around so I went home alone and it was a really lovely time. I set up my birth space, lit a beeswax candle, played music. I got into the shower and took my birth stool with me and just lay over it and had the water running on my back.
“I’d asked my instagram following about the TENS machine and the response was overwhelmingly positive so I hired one and put it on. I was mindful of staying active but not overdoing it. At 8pm we called the midwives and at 9:30pm we called again because labour was intense and I was getting strong hip pain. She suggested I get back in the shower which felt like more relief than the TENS machine could give me at that point. I was in the shower till midnight and by that stage my midwife was with me.
“When my waters broke I was really vocal and my midwife was squeezing my hips – it’s amazing how much relief that gives you. I got in the birth pool and did a lot of passive pushing – I wasn’t active in that process at all. This went on for a while and my midwife checked me and told me his head was right there. I sat on the toilet to use a bit of gravity which wasn’t comfortable at all, hence I knew it was effective. I got back in the pool and I birthed his head and could feel his shoulders wriggling. It was amazing to know how active he was in the process.
“My midwife helped me bring him out of the water and it was so special to learn that he was a boy. I felt so grateful and I just kept saying: ‘my baby, my baby’ – it was the most beautiful moment. I sat on the toilet to try and birth the placenta but the cord was quite short so I was hunched over. He was a big boy at birth – over 4kg – so he was heavy and hard to hold so we cut the cord once it was white and my husband had skin to skin.
“I had a quick shower and got into bed. Mali latched on beautifully and I could hear him swallowing. I see in hospital all the time that babies and mums come back from recovery and there’s already significant nipple damage so I was very mindful to get his latch as deep as possible.
“On day four my nipples starting getting quite sore and I had some pinching so I went to see Dr Amber Hart who was so reassuring. She got my latch feeling much better and gave me permission to take pain relief and rest my nipples. I needed that; I didn’t have to be a total martyr and it was nice to hear that from her. We worked on his positioning and I saw her again a few days later and after that it shifted and it’s been really comfortable ever since. Reassurance is so important in postpartum because you really do have days when you question yourself.
“At four hours post-birth I noticed that Mali was nasal flaring – he was working hard to breathe which is a sign of respiratory distress. The midwife checked his oxygen levels and they were below where they needed to be. We took an ambulance to Sunshine Hospital and they told us he had fluid on his lungs that needed to be pushed out and that was preventing him from taking those really deep breaths. He stayed in NICU for 36 hours and I was admitted as a postnatal patient. It was very overwhelming and we felt really anxious even though there were reassuring signs that he would be okay.”
You can connect with Joelleen over at JWP

Topics Discussed
Breastfeeding, IBCLC, Midwife, NICU, Physiological birth, pregnancy loss, publicly-funded homebirth, Waterbirth
Episode Sponsor
Today’s episode of the show is brought to you by my online childbirth education course, The Birth Class.
What makes The Birth Class so unique?
Well, instead of learning from one person with one perspective, we’ve gathered nine perinatal health specialists to take you through everything you need to know about labor and birth.
Realistic information is key to thorough preparation.
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us






