Podcasts Chloe – Induction, epidural postpartum planning
EPISODE 406
Chloe – Induction, epidural postpartum planning

In today’s episode, Chloe explains her choice to have public hospital pregnancy care so she could spend money on allied health services in postpartum. It was a choice that served her incredibly well as she had significant breastfeeding challenges and opted for at-home support from a GP + IBCLC specialising in perinatal health. Towards the end of her pregnancy, Chloe had multiple scans to check her baby’s growth and when an induction was suggested, she used the BRAIN decision-making model to assist her. Despite the fact that her labour and birth wasn’t what she planned, she felt like she had agency every step of the way and looks back with fondness on her experience because she felt heard, respected and supported (the foundations of a positive birth).
“Felix is almost five months now. On the one hand I feel like it’s flown by but on the other I can’t imagine a world without him in it. We’d decided that we wanted to have at least one child and I thought it would take a really long time to get pregnant so we were trying but not really trying and then six weeks later I was pregnant. I definitely had to get my head around that fact.
“Generally I didn’t ask pregnant friends about hospital options and models of care when they were pregnant so it was only when I found out I was pregnant I was really starting from the beginning. I saw a GP to confirm the pregnancy and then I started a relationship with a good GP after that. I wanted to go public and save money for things that might come up postnatally. I thought it was a better way for me to spend money than paying for private hospital care. I’m really glad I made that decision.
“The birth centre at RPA gave me a call and they explained that it was for low-risk pregnancies and ideal for people who weren’t planning on having an epidural. I sat with it for a few days but the more I thought about it I felt like it was my goal to have a physiological birth and it was a really good decision; the midwives were so wonderful. We also got home visits for two weeks after birth and that was so appealing.
“In my second trimester I got covid and I was coughing persistently which really affected my pelvic floor. I went to see a women’s health physiotherapist and that was a game changer for me; she was terrific and really helped me throughout pregnancy and postpartum and helped me gently get back into exercise after birth. The one thing I wish I’d done in pregnancy was more breastfeeding preparation. I came across Dr Eliza Hannan and she visited us in the home and it was such a pivotal point in my postpartum experience.
“I was so glad I had a pool of money aside so I didn’t have to worry about the financial burden of seeking support from a lactation consultant on top of the stress of breastfeeding challenges. When everything felt stressful, I was really grateful that I’d put the money aside for postpartum support; it was a thousand times worth it.
“The third trimester was the best for me; I had heaps of energy, I felt like I could still move around really easily, I was doing yoga and swimming a lot. Towards the end I had a scan where they noticed that Felix’s stomach was quite small and I ended up having weekly scans and they created a lot of anxiety and threw everything into a tailspin. They were worried about the functioning of the placenta and that he may have been growth restricted but still now I don’t really know what it was. He was and still is a small baby, that’s just how he is.
“I was on alert that I may have some anxiety postnatally because it wasn’t new to me and it really ramped up during all the scans. It was still pretty tough and I felt a real sense of responsibility to monitor his movements and recognise if something was wrong because no one else could do that for me. I went up to the birth centre a few times concerned about his movement; it was just weighing really heavily on me and perhaps more than I was acknowledging. I was so relieved when he was born and there were other people checking up on him and reassuring me.
“I really wanted to go into spontaneous labour; I was really worried about having an induction and of course I ended up with one. It was a discussion with all the scans I was having. I felt really confident about labour and birth throughout pregnancy but when the scans became regular so too did my anxiety about labour.
“I was 39 weeks when I went into hospital to check his movements and they asked me to come back the next day for a scan. It was then that they suggested an induction. I’d done a Calmbirth course and learnt the BRAIN method (Benefits, Risks, Alternatives, Intuition, Nothing) so I went home to really think about it. I went into the birth centre the next day and I went in and they were just wonderful. One of the midwives sat with me for almost two hours, talking through the induction, reassuring me that my midwives would still be involved. I went home and acknowledged that I was just getting too anxious and the induction was booked for Monday morning.
“I like to know what’s happening and have a plan and knowing the steps of the induction was really helpful. They started by inserting the gel and I was still able to walk around the hospital grounds. I had mild cramps but nothing serious. That evening they checked me and I was 1cm and it was so crushing. In the middle of the night, I had to have the foley balloon inserted and I don’t want to scare anyone but that was really hard. Henry wasn’t there so I was feeling really lonely. I went back to my room and that’s when the contractions were ramping up. Henry came back at 6am and that’s when I was moved to the birthing suite.
“Once I got in there, I was deep in labour. I had the CTG monitoring on so I couldn’t get in the bath. It became a very medicalised, hospital experience very quickly. I had also tested positive for GBS so I also had the antibiotic drip and that was put in as soon as I got on the birthing suite. I was on all fours on the floor but also moving around, standing up, leaning on the bed. The CTG monitor just kept falling off and it was so frustrating. I deal with pain by moving and Felix’s heart rate was doing funny things so they really needed to monitor him.
“I look back on the whole experience with a lot of joy even though it didn’t go the way I wanted it to. There was a stage when I just felt like I’d lost my confidence and I just couldn’t do it anymore so I opted for an epidural and I’m glad I did because I was distraught; I couldn’t reel myself back. But then the epidural was a wave of relief and without the physical pain I was able to think clearly. They were testing his lactic acid levels through this test but the OB said I could risk
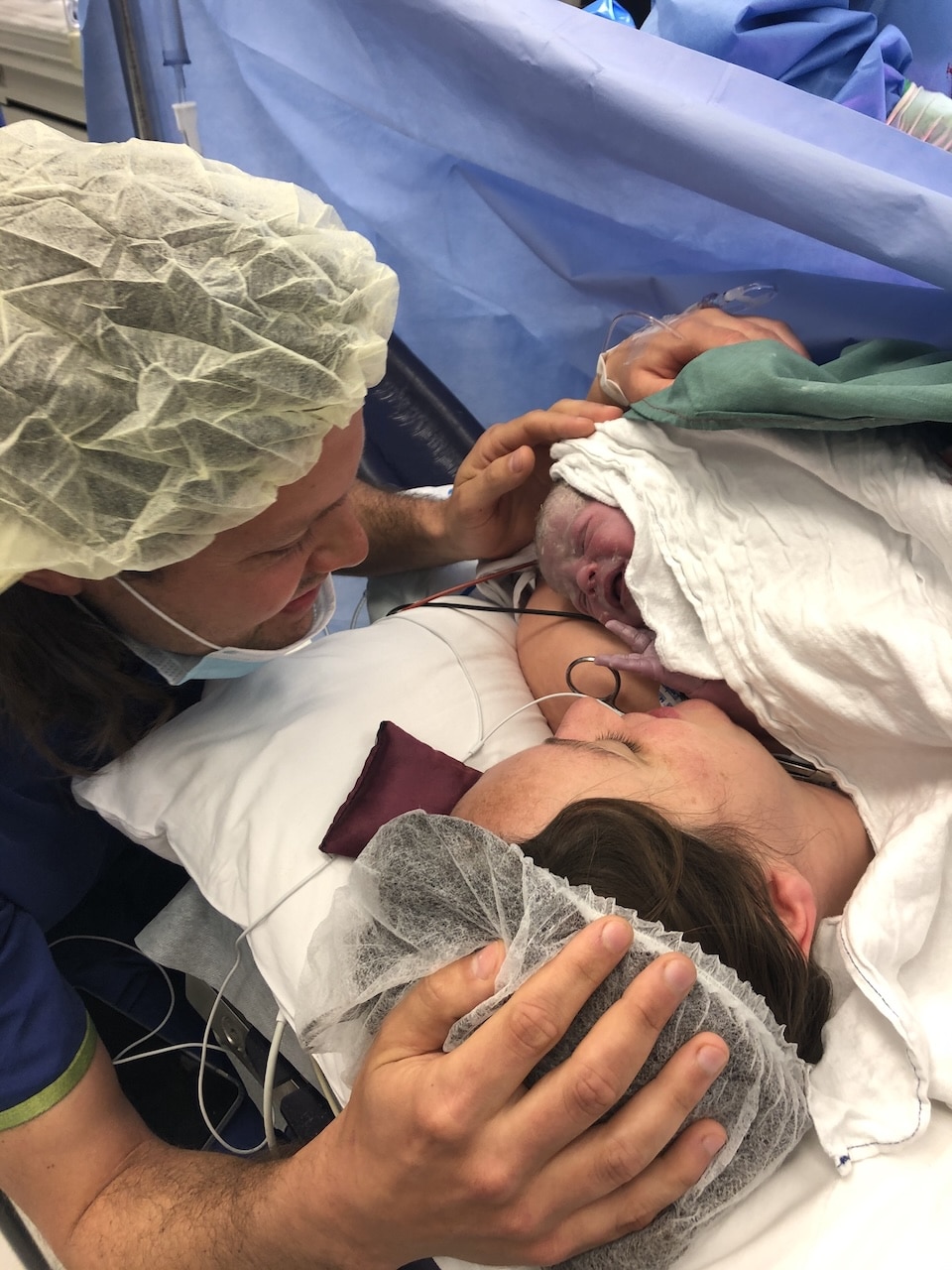
“They suggested an emergency caesarean and I was fully prepped and I was in the operating theatre. They looked and then Felix’s head was right there and they asked me if I gave them consent to have an episiotomy and forceps. I was so numb but the midwife I had was able to give really specific instructions which definitely helped. Felix cried immediately and was wide-eyed and perfect. That little moment is the most vivid from the whole experience. Even though things didn’t go the way I hoped, I definitely felt like I had agency the entire time. I felt like I made all of the decisions so I’ve been able to sit with it because of that. I don’t have any regrets because I made the decisions for a reason.
“Felix was on my chest straight away and I was taken up to a private room which was very lucky. I stayed for three days which was longer than I anticipated. Felix was small (2.9kg) and had jaundice but they never had to use the lights or get a blood test. I was eager to get home at the end but I’m also grateful that I had that time because it really helped my recovery.
“When we were home, the midwives visited and it was a game changer. Healing from an episiotomy was pretty rough; I was shocked at how hard my physical recovery was…I could barely walk around the block. I was swollen and really sore. At 11 days I wondered if maybe I had an infection so I went into the birth centre and they weren’t really sure but gave me antibiotics anyway. While I was there they weighed Felix and he wasn’t on track to regain weight. He’d been latching fairly well but it was also difficult to get him to latch so they were concerned about how much milk he was getting. They showed us how to triple-feed and that was an ongoing journey. Every three hours I would feed, pump and top-up feed him with either formula or breastmilk.
“It took a lot of reading, talking to midwives and friends to accept the transition to formula and it felt really challenging. Every decision you make feels so weighty; it’s stressful and you’re sleep deprived and you want to do everything that’s best for your baby. For everyone that’s done triple-feeding they know that it’s such a uniquely difficult challenge. At about five weeks I got in touch with Eliza and she is a total expert and she got it. She was so reassuring and gave me my confidence back and slowly we’ve weaned off the top-ups and now we’re primarily breastfeeding.”



Topics Discussed
Birth centre, BRAIN, Epidural, Episiotomy, Forceps, Induction, One baby, Postpartum care, triple-feeding
Episode Sponsor
The Birth Class is an online birth education course that helps you confidently prepare for a positive birth experience.
Featuring 10 audio lessons with perinatal health specialists, you can listen from the comfort of your home when you’re relaxed and receptive to new information. The Birth Class is a conversation starter between you and your birth partner that informs, encourages and empowers you to journey towards labour with knowledge and confidence.
Categories
Related Products
-
The Birth Class
108 reviews$249.00The empowering online childbirth education program that will help you confidently prepare for birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us