Podcasts Jayne | Postpartum – homebirth, breech, planned caesarean
EPISODE 447
Jayne | Postpartum – homebirth, breech, planned caesarean

Whilst many people think that organ donation is dependent on the information on your driver’s licence, you actually need to officially register as an organ donor. You can do that at donatelife.gov.au
“At heart I’m a homebirth mum, I’ve kind of taken that on as part of my identity. My first two pregnancies were a dream and we decided early on that the homebirth route felt right for us. We met our homebirth midwives and they’ve stayed with us throughout all three pregnancies; they feel like really special aunties; they’ve been absorbed into our family which is really special.
“My first birth was a homebirth hospital transfer; I laboured at home but there were a few reasons why we needed to get to hospital. We came home after a few hours and I got into bed with my newborn. In hindsight I had a really soft landing into motherhood. My second birth, three years later, was my healing birth. I laboured for a really long time – all up close to 48 hours – and I had a doula who was with us throughout. It was the picture perfect homebirth; my second son was born on the lounge room floor, there were fairy lights and the fire was roaring. It was beautiful. It was incredible to know my body could do that; I felt like I really stepped into my birthing goddess power and really claimed it.
“When I conceived my third son, I just envisioned another birth like my second. At around 28 weeks we discovered my baby was breech but I knew he had plenty of time to turn; I did all of the things. I read every piece of information about turning a breech baby; I was doing inversions, pressure points, and I stuck a peppercorn to my little toe. I was really determined because I had a really strong vision of having a homebirth. One of my midwives kept telling me that babies are often trying to tell us something when they’re breech.
“At 36 weeks he was still breech. I went for an ultrasound in preparation for an ECV and I went down all the rabbit holes of googling that which is never a good idea. My doula came with me and thank goodness she did. The sonographer left the room and told me he was checking something with his supervisor. He came back and mentioned there was an issue with my baby’s kidneys and I was sent to the hospital where the obstetrician mentioned that there was too much fluid and I needed to go to Hobart.
“It didn’t feel real; in fact 10 months later, it still feels surreal. I went home and two days later we made our way to Hobart to see the specialists. He has a textbook case of posterior urethral valves where a little bit of skin blocks underneath the bladder so the urine backs up and then fills up the kidneys. I was 36 weeks at this stage and my amniotic fluid was really low which is problematic for lung development as well.
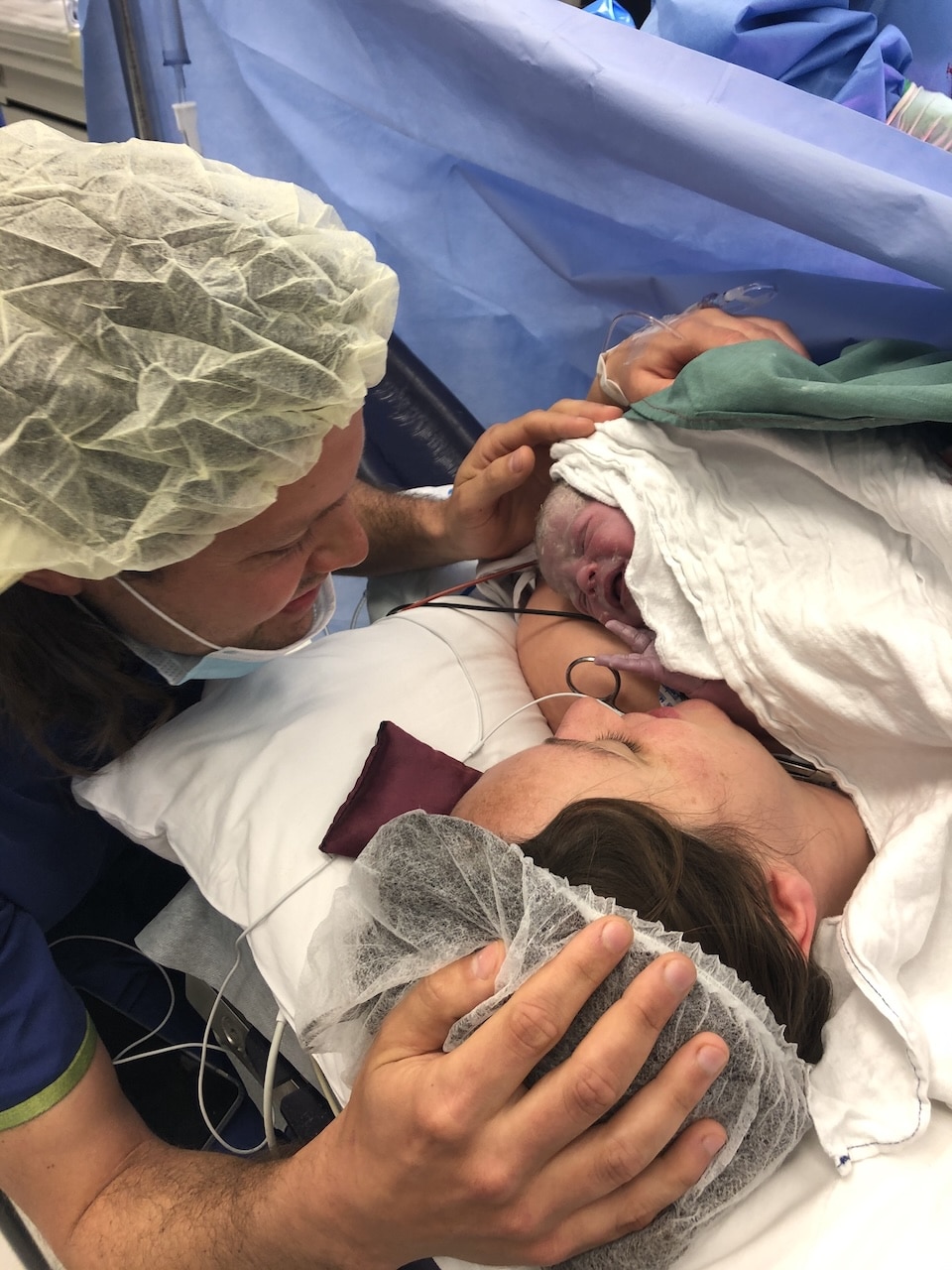
“There was nothing I could do, I just had to roll with it; that’s been the theme from then on. My sister came from New Zealand for a month and it makes me weep when I think of what she did for us and the boys, she was just there to hold us all. I went into labour a few days before my planned caesarean and on the day, I really felt like I couldn’t engage in it, I felt like I just had to get through it. When he was born they put him on the top of my chest near his shoulder. He was crying but he was quite purple and soon after they took him to NICU.
“My blood pressure was really low so I spent four oblivious hours in recovery, wondering what was happening to my baby. I remember I was waiting in my room before the caesarean and telling my husband to get the little bonnet and special clothes out and the midwife telling me that we wouldn’t need them…there’s so many weird little moments like that…so much normal gets completely wiped out. In the first few days, when you usually announce your baby’s arrival and you say that mum and baby are doing well….I knew I couldn’t write that because neither of us were doing fine. All those normal little things which you don’t get, you get something else.
“The first night I was in bed, I couldn’t move, there was an empty bassinet at the end of my bed. Beside me was a mother who was also a maternal child health nurse and neither of us could sleep. It was her night two so her baby was unsettled and I could hear the pat, pat, pat and I remember being so comforted by that noise, by the mum who got to pat her baby’s bottom.
“Eight hours after I’d given birth the paediatrician came in, introduced himself, and told me he’d been with my baby since birth. He told me words I’ll never forget; that my baby was sick but safe. It was so strange; it’s still so strange. That’s when I found out about his lung issues- he’d had a pneumothorax which is where air collects outside the lung and causes the lung to collapse. Later that night another paediatrician came to tell me that he had another pneumothorax on the other lung. I felt so disconnected; I didn’t even know what my baby looked like. I knew that I’d birthed him and I loved him and he was mine and he existed, but it was a foreign concept that I’d had a baby. I was lying in this dark room by myself, I couldn’t move or slow motion run to NICU like if I was in a movie, there were all these decisions being made without me.
“I was discharged at four days postpartum and stayed at Ronald McDonald House which was a 15 minute walk up a hill to the hospital, which wasn’t ideal considering I’d just had a caesarean. I’d only held him once and leaving the hospital without your baby is possibly the hardest thing I’ve ever done and I had to do it multiple days for the following month while he was in NICU. His lung issues were their priority and then they shifted their attention to his kidneys. When I was well enough to be with him the nurses started talking about expressing breastmilk; I had an oversupply for my first two babies so I was determined to breastfeed. I pumped every two-three hours overnight and took each bag of milk into the NICU every morning – 120ml from every breast which was far too much, the nurses joking that I could feed the whole ward.
“In hindsight he got better and better but in the moment, the day by day wasn’t quite as straightforward. He was in the ventilator and vibrating bed to keep his lungs open and he had so many tubes and interventions. At eight days old he had his first surgery to ablate the skin that was causing the blockage and that did the trick because started passing urine. He was tube fed and it became a bit of a battle to move over the breastfeeding but we got there eventually and soon after we came home. In NICU terms 26 days is fairly short but it didn’t feel like that at the time.
“Because of the damage that was done to the kidneys in utero, one of his kidneys doesn’t work and the other over-functions. He’s just had his fifth surgery and we know they’re not going to be solution but more of a maintenance service. Everytime there’s a new surgery it is progress but I also don’t really know what the answers are.
“I’m starting to get my head around the long-term ness of this. We will have to think about dialysis and transplants but for now we make sure he doesn’t get sick which is so hard with two big brothers who are at school. There’s a lot of travelling and health appointments and we just roll with it. He failed his hearing tests, like his big brother, so he’ll probably need hearing aids. There’s been so many tests and ultrasounds but in terms of today and his overall health, he’s the most glorious baby. It’s the biggest silver lining…a beautiful, beautiful child and I get to be his mum. It’s amazing. We happen to have the best village of people supporting us, too.”


Topics Discussed
Breech, homebirth, NICU, organ donation, Planned caesarean, posterior urethral valves, Three babies
Episode Sponsor
Today’s episode of the show is brought to you by my online childbirth education course, The Birth Class.
What makes The Birth Class so unique?
Well, instead of learning from one person with one perspective, we’ve gathered nine perinatal health specialists to take you through everything you need to know about labor and birth.
Realistic information is key to thorough preparation.
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us