Podcasts Lisa | Postpartum – two under two, MGP, posterior labour
EPISODE 442
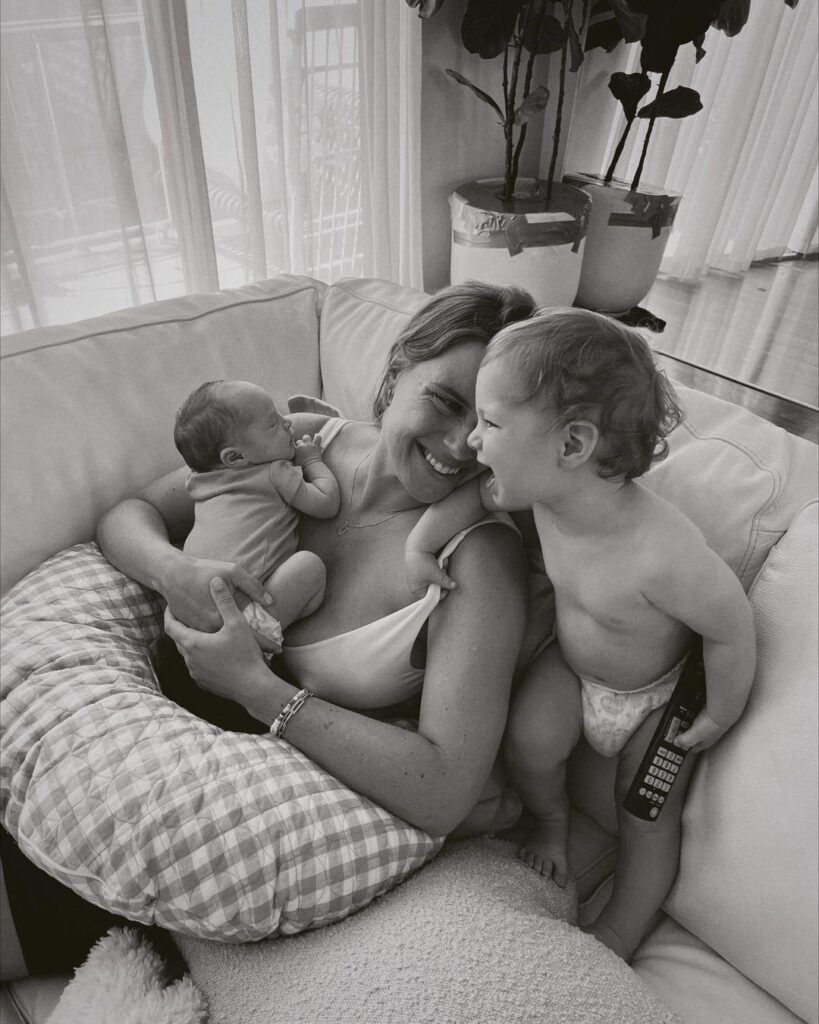
Lisa | Postpartum – two under two, MGP, posterior labour
“It took us eight months to conceive Fred. It doesn’t sound like a long time but it was covid lockdown and I was so focussed on my cycles and my dates…every time I got my period it felt like a stab in the guts. I just decided to not focus on it and I think I relaxed and it worked.
“I assumed I’d go with a private obstetrician but when I checked my cover I realised I didn’t have obstetric health cover. I was fine going to my local public hospital which was the Mercy in Melbourne. I come from a public health background as a women’s health physio and I knew about MGP and the great outcomes. It was actually very rare for me to see a woman in postpartum if she’d had MGP care. I also knew it was a model of care that was really hard to get into so I got my GP to refer me straight away.
“My biggest fear was having a third or fourth degree tear but it wasn’t an irrational fear. Continuity of care was really important for me; on the day I wanted it to just be me and my midwife and hopefully as little intervention as possible.
“Fred’s labour – from first contraction to last was 67 hours. I was in early labour for a really long time because he was posterior. It was four days before my due date and I knew straight away that it was a contraction. My midwife told me that I wouldn’t need to go to hospital till I was having three contractions in ten minutes and I couldn’t talk through them. I didn’t sleep much at all that night and the contractions didn’t get more regular till about 7am. I decided to get things moving so we went for a walk, I got on the gym ball, had the TENS machine on. By 6pm nothing much had changed so I watched Father of the Bride 2 and then it got to 9pm and I was emotional and so tired. Another day passed and my midwife encouraged me to get in the bath but by 5pm I felt like I needed to see her and talk to her. She encouraged me to come in and once I got there I got on the gas and it went through me like a cool breeze; I loved it. She did a vaginal examination and I was 2cm so she gave me the option to stay or go home and keep doing what I’m doing.
“I went home and I was in the shower all night. By 4am the next morning I was done, I just wanted to go to hospital. The contractions slowed down in the car and once I got there my midwife checked me and I was 6 cm which was great. I got in the bath and I got really zen; I put my affirmations on, Daniel was giving me water, there was music playing. I was loving the gas and feeling reasonably good even though I was exhausted. My student midwife was amazing, massaging me and supporting me. By 10:30 am I really felt like I needed something for the pain because the more exhausted I got, the worse the pain was. My midwife offered to break my waters and induce me with the syntocinon drip and then I finally got what active labour contractions were like.
“When it came time to push, Fred still hadn’t completely turned from posterior. At about 4pm his head was born and then his body but he wasn’t breathing. I knew code blue’s happened quite regularly on the maternity ward and I knew there was a high chance of it because I’d had two doses of morphine. The pediatricians came in and gave him oxygen and within five seconds he was breathing and screaming and he was fine. Eventually he came back to me but I was so exhausted I could hardly hold him. We stayed overnight and I was lucky enough to get a private room; I was so exhausted and thankfully he slept really well and so did I.
“My perineum was so swollen but this is where my background in women’s health physio kicked in because I knew I needed ice. I elevated my legs and wore recovery shorts and that support was incredible; it’s all soft tissue and muscle and needs to be held. I set my alarm to do my pelvic floor exercises; that’s always been my advice to my patients. The weakness after birth shocked me; I had all the clinical knowledge but the practical and personal experience was something else. I started doing light pelvic floor exercises about three days after birth and then I very gently and gradually increased as the weeks went by.
“When Fred started sleeping through, Daniel and I just decided not to use protection. I conceived straight away and Fred was only seven months old. I hadn’t even got my period back but I started feeling a bit different; my allergies were playing up, I felt really faint when doing hot pilates and Fred started pushing the breast away. I did a test and I was pregnant. I went to my GP and then got a dating scan and I was already eight weeks.
“I got into the MGP programme again and my midwife was amazing and had me doing all the spinning babies techniques to ensure I didn’t have another posterior baby and 67 hour labour. I was swimming, floating on my belly using pool noodles to float, doing all the things to prevent it. Labour started spontaneously but we were of the mindset that it would take a while. We dropped Fred at my in-laws and then returned home. I got in the bath and got the most debilitating contraction; I held onto the side of the bath and was frozen. This was about 11am and then they started coming fast and they were really intense. We got in the car and Daniel dropped me at the door, I was on all fours screaming. He got me in the lift, we went straight into the birth suite, I got on the gas, my midwife arrived five minutes later and she checked me and I was almost fully dilated. I got in the shower and the pain was so intense. Evelyn was born an hour after we arrived at hospital and as my midwife said, all that work to get her in an anterior position had helped so much.”

Topics Discussed
MGP, Physiological birth, Posterior labour, Spinning babies, Two Babies, two under two, Women’s health physio
Episode Sponsor
If you’re pregnant, we encourage you to start thinking about your birth recovery now. You need more support in the fourth trimester (the 12 weeks after birth) than you do in pregnancy which can be surprising to many new mothers. It’s for this reason that Bare Mum began and now they offer a beautiful collection of practical and supportive products to assist your postpartum healing.
All new mums need lower back, abdominal and pelvic floor support after birth. Bare Mum’s Postpartum Briefs gently hold you in the first days and weeks, helping you feel confident. Endorsed by the Australian College of Midwives, they offer a unique pocket design so you can insert a warm or cold pack to offer soothing relief and assist with caesarean wound or perineal healing.
Ideal for caesarean and vaginal birth recovery, Bare Mum Postpartum Briefs are soft, stretchy, and supportive, offering you essential post-birth care. They’re a must-have for your hospital bag.
Bare Mum is offering you 15% off storewide with the discount code ABS15
Categories
Related Products
-
Birth Combs: Harness Your Body’s Natural Pain Relief
$24.95Crafted from smooth, natural wood, our birth combs activate specific pressure points in your hands that trigger your body’s innate pain-relieving responses.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us






