Podcasts Tess | Postpartum – PPH, triple-feeding
EPISODE 434
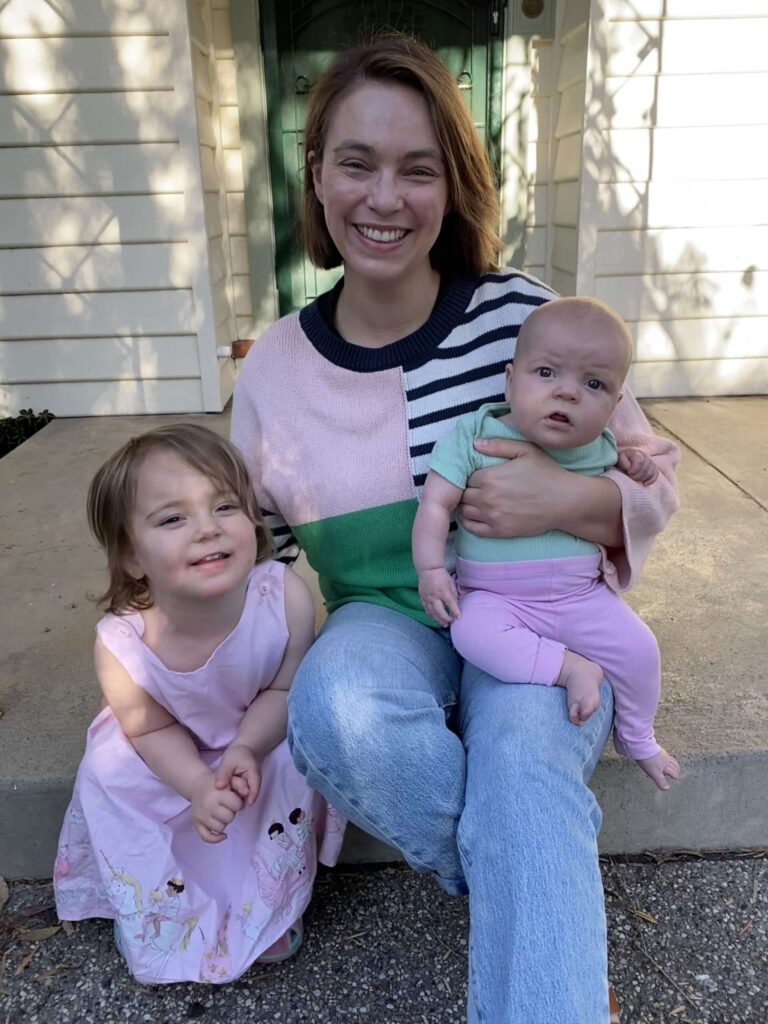
Tess | Postpartum – PPH, triple-feeding
“I had an unexpected induction at 38 weeks. I went in for reduced foetal movement and they found that both the baby and I had a high heart rate because I had a fever. It was a pretty nerve-wracking experience because the monitors were constantly going off. I ended up with a forceps-assisted birth which led into a postpartum haemorrhage so it was a difficult birth and a bit scary and I think it really affected me mentally and emotionally as I started my postpartum journey.
“I stayed in hospital for a few nights because they could see that I was physically and mentally struggling. One of the hurdles to getting breastfeeding established was that I always thought I was about to leave hospital; there wasn’t much communication about when I’d be discharged. I couldn’t relax into it and I was so terrified to take my baby home that I just focussed on the short-term solutions. Those experiences really shaped the rest of my breastfeeding journey.
“The midwives offered very good and well meaning advice but I was overwhelmed and depleted. They also offered home visits after discharge but it was still covid times and that effected the support I was able to access. One of the things that’s tricky with breastfeeding is that you may see someone for one feed and for every other feed you’re muddling at home by yourself. At that time it was also really hard to access specialist lactation support.
“It was always my intention to breastfeed but I was really lacking in confidence in my body’s ability to birth and breastfeeding. In the back of my mind there was always the niggling doubt and that’s undoubtedly unhelpful. I’d read a lot about breastfeeding and the physiology of it but I hadn’t accessed the education I think I needed. I also hadn’t built a relationship with a care provider in pregnancy and that informed my choices for my second pregnancy.
“I sustained nipple damage the first time she latched so right from the start I was dealing with nipple trauma and pain which made feeding in the following days really difficult. I was also really depleted and trying to rest as much as possible so my baby spent a lot of time in her bassinet and was brought to me to feed and by the time she was with me she was screaming which made it even harder for her to latch because we were both stressed. The hospital midwives taught me how to hand express so I expressed into syringes for the first few days and after that I started trying to get her on the breast.
“She lost 11 percent of her birth weight so that’s when I started triple-feeding; feeding a bit on the breast, topping-up with formula and then I would pump to continue the stimulation of the breast. It was completely exhausting with every session taking roughly ninety minutes and she was on three-hourly feeds. My partner and I were both up during the night because while I pumped he was feeding her the bottle so we were both wrecked. I didn’t realise at the time that triple-feeding is supposed to be a stop-gap option, you’re not expected to continue with it long term.
“On day 4 we had a home visit from the hospital midwife and she thought my breastfeeding looked good and she encouraged me to give up the triple-feeding. I was using nipple shields and in retrospect I think they may have been inhibiting milk transfer. We tried to move back to exclusive breastfeeding and I thought it was going okay I was happy to not have to pump. The next day we went to hospital for an appointment with the lactation consultant and she didn’t think my baby looked right as she was very lethargic and sleepy. We saw the pediatricians and spent the day in special care and they really emphasised the importance of getting calories into her so they recommended bottle feeding.
“At that point I was devastated that there was something wrong with my baby and I hadn’t realised. I feel incredibly guilty that I’d stopped triple-feeding and thought everything was going well enough. It’s such a huge learning curve, learning to feed, learning to do everything. It took me a long time to get past the guilt of that. We were on a three-hurly feeding plan and I did exactly what the paediatrician recommended so I stopped breastfeeding at that point so I did what I knew would work. I was exclusively pumping so my partner would bottle feed her while I pumped. I really missed out on that bonding time with her because she would sleep as soon as she had fed.
“I pumped for her for over 12 months and it meant I wasn’t able to live my life in the way I normally do because I would be feeding and pumping and by the time I’d washed and sterilised all the bottles and we were out the door I’d have to be back home within 90 minutes. I never got the hang of pumping on the go so I did feel tied to home. It was really isolated, both from a logistical perspective but also I didn’t know many people who exclusively pumped, although there was another mum in my mother’s group and we really connected over that experience.
“After Harriet regained her birth weight at two weeks old, my child health nurse encouraged me to get her back on the breast, reassuring me that Harriet would tell me when she was hungry and if she was getting enough and wouldn’t become that lethargic baby again. I started looking for lactation support so I had guidance on that journey but that same week I had a secondary postpartum haemorrhage at home and was transferred to hospital in an ambulance. I ended up having retained placenta and I was scheduled for a D+C three weeks later; it was such a hard start. That was the last straw for my mental health because I went into full blown survival mode. “I really froze inside and had a lot of anxiety. My intention was to just keep everyone alive so pumping was predictable and containing and it was giving me a focus and a way to care for my baby.
“We knew we wanted a second baby and we conceived much sooner than we predicted. I chose a different model of care and opted for a private obstetrician which was the foundation to a much more positive start to postpartum. I was diagnosed at 32 weeks with gestational diabetes and I was expecting a bigger baby so I elected for an induction of labour because I didn’t feel comfortable going into spontaneous labour or labouring at home because of my secondary postpartum haemorrhage experience.
“Breastfeeding was a focus very early on in pregnancy for me. My heightened anxiety meant I needed more intensive support so I was looking for residential stays because I knew an hour-long appointment with a lactation consultant wasn’t going to be sufficient. I found DR Amber Hart who runs a clinic in Melbourne and I had an antenatal appointment and education class with her that were really helpful in building my confidence. The really amazing part of the clinic is the breastfeeding day stay where all of your feeds are supervised and you get to see a range of professionals to support you on your postpartum journey. It’s the service I so desperately needed the first time around. I knew when I would be birthing so I booked the day stay for the day after I was discharged from hospital. The longer stay in the private hospital was also a benefit because my milk came in while I was in hospital and my birth was quick and easy; I was euphoric. I was more relaxed in general about letting her come to the breast and just observing her. It felt really different and she had a good, long first feed at the breast. Over the next few days I saw so many midwives and they all had different opinions and techniques and while that was confusing, I was comforting in knowing that they were checking on my baby and would notice if she wasn’t getting enough.
“I couldn’t express colostrum after birth so I completely catastrophised. I was really nervous about the prospect of having to start triple-feeding but I was also so comforted knowing that I had the day-stay booked. It’s the most amazing service and if it’s the future of postpartum care it’s so exciting. I had a one-hour consultation with Dr Hart where she weighed my baby and observed a feed and it got me sorted immediately from a comfort perspective. Then you move into a day spa that’s set up for mums and babies and there’s reclining chairs. They also have a mother’s helper who served me tea and fruit and all day there’s someone on hand to help you. I also saw a physio and sleep consultant and had a massage so I felt so nurtured and it makes learning so much easier when you feel like all your needs are being met. All of your feeds are supervised by Dr Hart, giving me tips and helping me get established. It meant that on day 5 I was having pain-free breastfeeds and it completely changed the game for me.
“The day stay is subsidised by medicare and while it’s not cheap, it was so worth it. I was so desperate to breastfeed because I had a lot of grief and guilt after my first experience and I worried that it had affected my attachment with my daughter. But I really believe that the best way to feed your baby is the way that works for you.
“My second postpartum has been really healing for me and now that I’ve got the comparison, I can look back and see that I wasn’t in a good way and I was doing my best and I’ve forgiven myself. I’ve got so much more time now to spend with my girls. I am sad that much of my first year was marked by grief and guilt but I’ve got a gorgeous, hilarious, cheeky toddler now and I am absolutely loving this stage of motherhood.”

Topics Discussed
EBM, PND, postpartum day-stay, PPH, Private obstetrician, triple-feeding
Categories
Related Products
-
Birth Combs: Harness Your Body’s Natural Pain Relief
$24.95Crafted from smooth, natural wood, our birth combs activate specific pressure points in your hands that trigger your body’s innate pain-relieving responses.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us






