Podcasts Maria – twins, bed rest, IUGR, caesarean birth, NICU
EPISODE 441
Maria – twins, bed rest, IUGR, caesarean birth, NICU

“I had a history of PCOS and my GP recommended I see an obstetrician but I didn’t feel like I had a good connection with him. A few months later a friend recommended Lynn Burmeister and she was really open and shared our options with us. She recommended ovulation induction because my periods were always irregular. We started the process and it only took a month for me to fall pregnant but I was never expecting twins.
“Three days before my scheduled 8-week scan I had some cramps and I was so scared of miscarriage that I called the clinic. They encouraged me to get an earlier scan and that’s when I found out I was having fraternal twins. I was nauseous and tired all the time but it definitely wasn’t really bad.
“After my 20 week scan my obstetrician told me that my cervix had shortened significantly and I was at high risk of having the babies within a few days or weeks. She booked me in for a cervical stitch the following day and told me to go home, pack a bag and come straight back to the hospital. I was put on bedrest with my legs elevated and could only get up to go to the toilet. I just wanted my mum and the language barrier was a bit of an issue, especially when talking to the midwives. I’m quite positive in nature so I just decided it was going to be okay. The surgery went well but not as well as she had hoped. I also had excess amniotic fluid which wasn’t ideal because it was creating extra pressure.
“I was really stressed and scared till 24 weeks but I also felt that my pregnancy would have a happy ending. Mindfulness and meditation allowed me to remain in the present and take it one day at a time. I know it’s the role of the obstetrician to tell me about the risks but it’s not always helpful because it creates so much fear and anxiety. I was going to do everything in my power to get a good outcome for the babies. I also found so much comfort in friends who had similar pregnancies in their pregnancies. I journaled to help process my feelings and I had weekly goals and projects to keep me busy, including hiring a German teacher who came to the hospital twice a week as I’d always wanted to learn German but had never had the time.
“I felt like my body, mind and soul were really connected to get towards the end of the pregnancy. The boys were growing consistently till week 29 weeks but then they slowed their growth rate and Emily started to get concerned. At the start of week 33 I noticed that one of the twins wasn’t moving as much. I was still on bedrest but going from home to the hospital was stressful. That was when Emily told me it was time for the boys to be born.
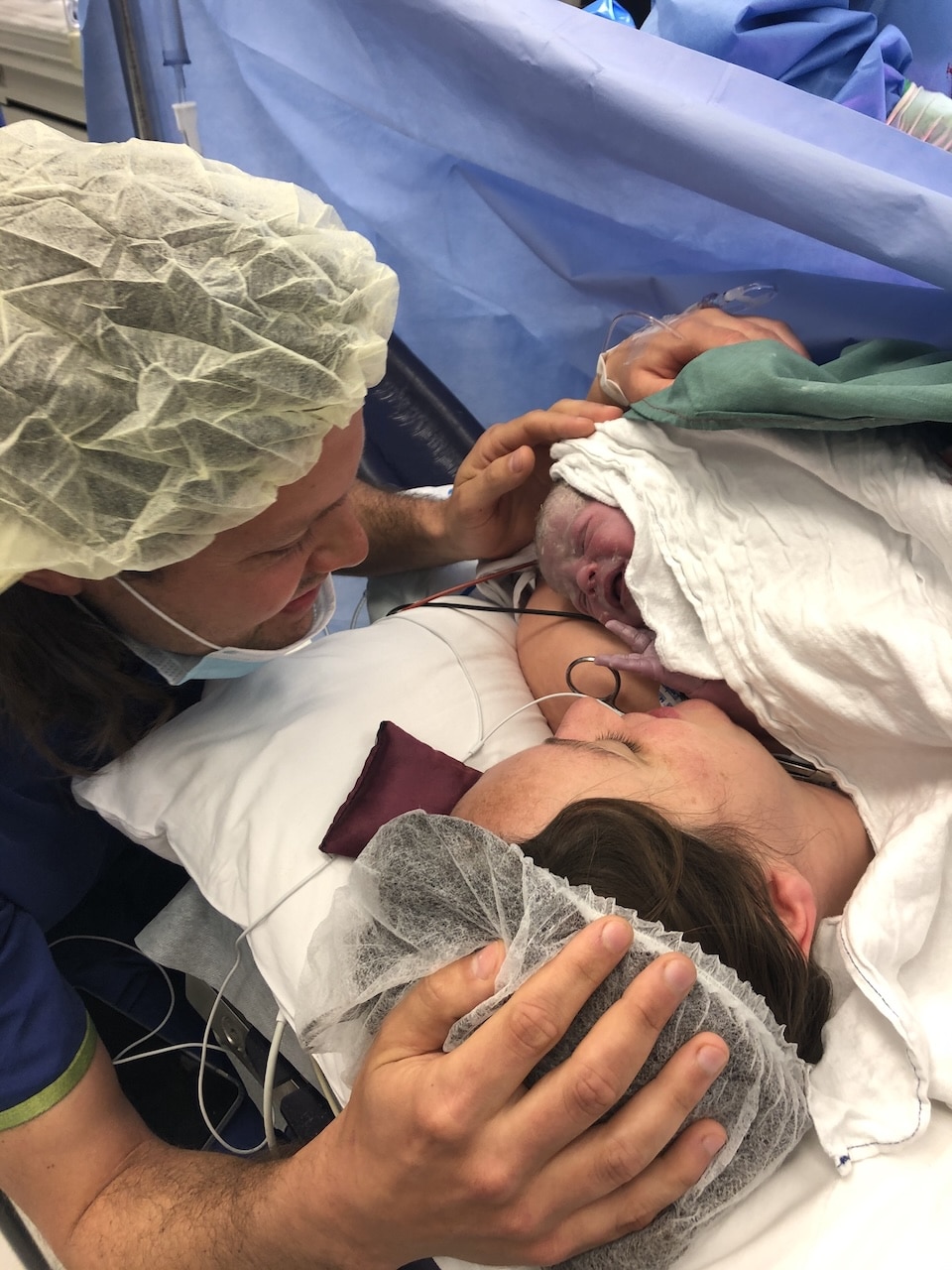
“I had a planned caesarean and there were about eleven people in the room. They put the boys on my chest for a few seconds and then immediately took them to NICU. They told me they were doing well and they kept me informed. I went to NICU later that day to see them but we couldn’t take them out of the incubators. A week before they were born Emily had taken us to the NICU to show us what to expect and that definitely helped.
“I was discharged after five days and it was a huge relief to be able to walk after 14 weeks of bedrest. It was a slow process but I was just happy to be able to be independent again. But yes, I definitely felt sad being away from the boys. My mum came from Colombia to help and it was so lovely to have her. The boys came home after six weeks and my mum was there and she helped us a lot. I could sleep during the day. The NICU was great training and the nurses and midwives gave me so much confidence but it was hard to stick with the routine that had been established. But I was so grateful for everything, especially after a high-risk pregnancy, it really helped with the tiredness and sleep deprivation. I also had volunteer help from Caring Mums and the Australian Multiple Birth Association (AMBA) which was so helpful.
“The boys are now four and speak German, Spanish and English. We stayed in Colombia for eight months because we got stuck there during covid and then we went to Germany for six months because Australia’s borders were still closed. It ended up being a wonderful opportunity for us.”
The organisations that helped Maria along her journey were: The Australian Multiple Birth Association and Caring Mums
You can connect with Maria over at Nurtured to Bloom Nurtured to Bloom is a platform where women facing complicated pregnancies can find emotional support, mentorship and connection to navigate their pregnancy journey with acceptance, self-trust and determination.

Episode Sponsor
Today’s episode is brought to you by my online birth education course The Birth Class.
Featuring 10 audio lessons with perinatal health specialists, you can listen from the comfort of your home when you’re relaxed and receptive to new information. The Birth Class is a conversation starter between you and your birth partner that informs, encourages and empowers you to journey towards labour with knowledge and confidence.
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us