Podcasts Amber | Postpartum
EPISODE 408
Amber | Postpartum

Listen to Amber’s full birth story in episode 391 here.
From 36 weeks onwards I did regular antenatal expressing so I had lots of colostrum stored in the freezer ready to go and I had a breast pump and silverettes on hand in case I needed them in the first few weeks of postpartum. As a midwife and IBCLC had all the knowledge on board so I didn’t do any education although it’s something I strongly suggest to women in the final weeks of pregnancy; get educated about breastfeeding so you’re prepared for the practicalities. I also had a lactation consultant ready to go in case I needed that professional guidance and I had an in-depth postpartum plan to support my breastfeeding journey which included a freezer full of food for nourishment and the intention to rest.
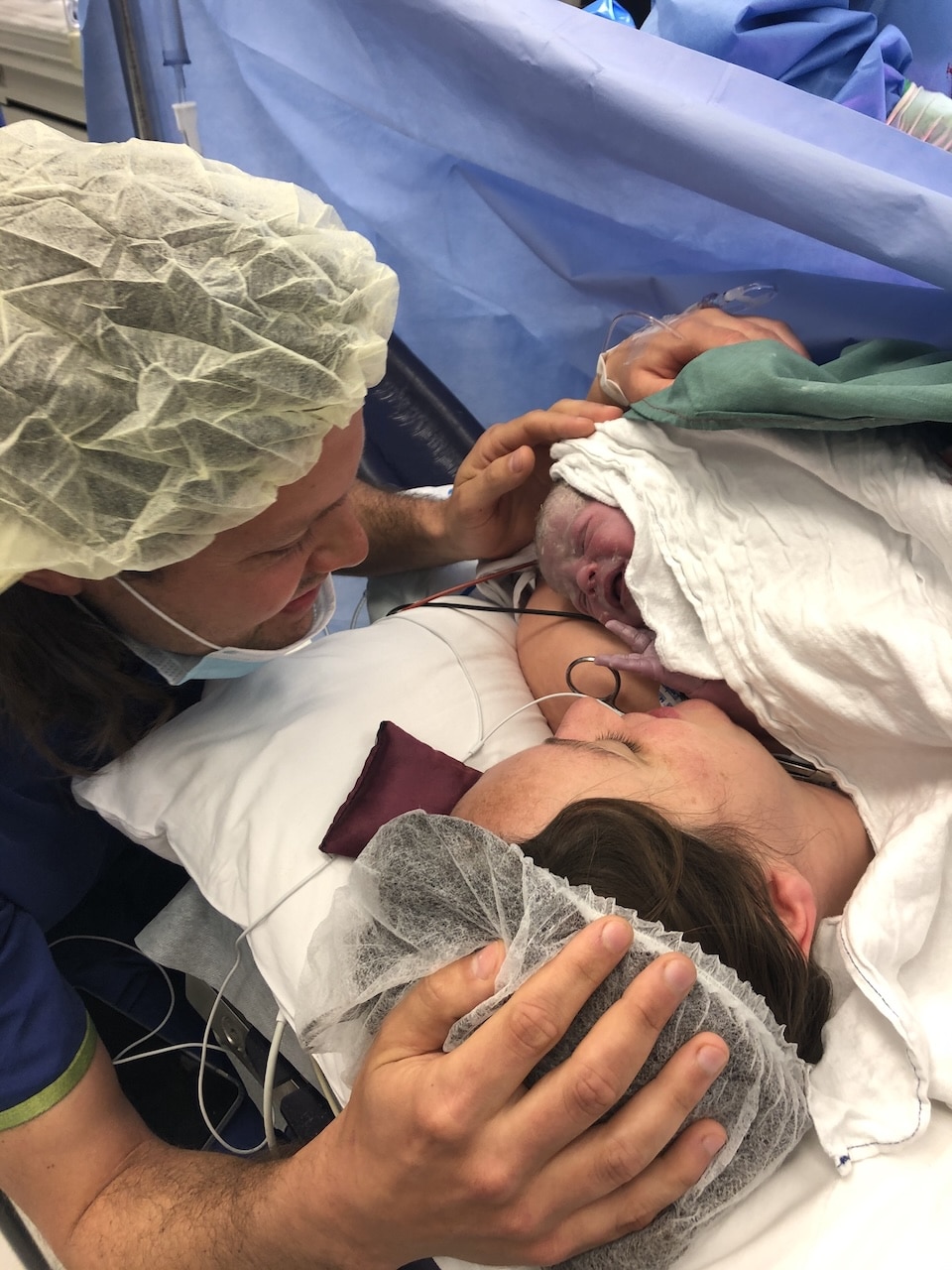
When I spoke through my birth plan with my doula it was very important that no one put the baby on my breast after birth. For me, one of the most important parts of birth was the breast crawl; I wanted my baby to have the chance to lick and suck around. I’ve spoken about the breast crawl in my antenatal education for years but unfortunately for me, it didn’t happen because I was haemorrhaging and my baby was separated from me and then when she came back to me, I had to latch her straightaway to help the uterus contract. I knew it wasn’t a good latch but I had to get her sucking to assist with the contractions. She did a breast crawl the following day which is good for people to know; if you’ve had a traumatic birth and things haven’t gone like you envisioned, you can do these things later on.
I knew a traumatic birth and blood loss was a recipe for delayed milk supply but I didn’t think it would happen to me. I thought my milk would come in easily and it definitely did not. In the first 48 hours I would try and get her on but her latch was shallow, chompy and painful and I’d have to get my little finger in there and take her off so we could try again. She wasn’t able to tilt her head back and go up and over onto the breast; her neck and mouth was stiff from birth and she wasn’t able to open and latch. My frozen stash of colostrum satiated her and then to stimulate my milk production I would hand express and thankfully I had a really good supply of colostrum so that kept us going.
I wore silverettes continually for two weeks. I’d been told they promote fast healing because silver is antibacterial, anti-inflammatory, antifungal and antimicrobial and the silverette creates space between the nipple so there’s no friction. I was shocked at how well they worked to heal my nipples which were cracked and blistered and they’re definitely something I will encourage all new mums to use in my work as a lactation consultant.
My midwives came to see me at home and on day 2 Winter lost 9.6 percent of her birthweight which was okay because it was below the expected 10 percent. Around that point she started latching and while it wasn’t my standard of a perfect, deep latch, I was happy with it. She was feeding well and for a long time and I knew she was bringing my milk.
At 4am on day 4 I was beside myself because I had a gut feeling that she hadn’t gained weight and while she was cluster feeding my milk still wasn’t in. Just before the midwives came that morning I felt a fullness in my breasts for the first time. I thought: Oh my gosh, I think my milk is coming in but I didn’t have a chance to feed her before the midwives weighed her. Winter had a weight loss of 12 percent which was a decent amount for a 4.2kg baby so the midwives contacted the paediatrician and that’s when I became concerned about being readmitted. The paediatrician said we could stay at home because otherwise she was well – there was no jaundice so she was really pink, she was waking for all her feeds and she was having wet nappies. The paediatrician recommended another weigh in after 24 hours along with 2-3 hourly feeds and 30ml formula top-ups. The paediatrician didn’t mention expressing at all so unless I knew the importance of it, I wouldn’t have done it and it was such a crucial step in bringing my milk in.
Winter was waking 2-3 hourly so I fed her, pumped after feeds and my milk was transitioning at this point. I only had to give her two top-ups of expressed breastmilk and the next day she had gained 120 grams which is a huge weight gain. I’m so grateful I could focus on her weight gain but also on my breastfeeding journey and make those decisions for myself that were right for our circumstances.
With the challenges I had, if I didn’t have the knowledge I had, breastfeeding may not have worked for me. It was knowledge that helped me get through the challenges. We know that over 90% of mothers start breastfeeding and then that statistic significantly drops because there’s so much conflicting advice and not enough support.
My breasts weren’t hard or soft; they were firm. I was taking anti-inflammatories for birth recovery and to try and help with breast inflammation, I used the flower-shaped ice-packs which I loved and I wore them constantly. Just before she fed I would hand express a little bit of milk which was helpful because I had a fast letdown and it softened the areola as it was so firm that she couldn’t latch. I did very gentle stroking while she was feeding and once she was finished I’d put the ice packs on. In the shower I did gentle reverse stroking from the areola to the armpit and I was drinking lots of water to encourage the engorgement to go down. That’s when I realised I had a lot of milk so she couldn’t drain my breast. She’d get on the breast and gulp and fill up so quickly so I’d get up, change her nappy, give her some time upright and then put her back on that same breast to drain it. My milk would spray for a a metre so I had a fast letdown too so hand expressing into a burp cloth before she latched on so I could get that initial fast letdown over so she could then latch and feed without coming off and choking.
I had to really heal from my birth and horizontal rest was essential for me, as it is for all women in postpartum. I couldn’t feed out and about which forced me to rest in the first few weeks. One of the biggest contributing factors to successful breastfeeding is the support around the mother. Not one person ever said; is this the right fit for you? Do you think you should try formula – they knew how important it was for me and they helped me through it. Support is integral to breastfeeding.
At four weeks it all came together for me; I’d recovered from my episiotomy, my breastfeeding was going well, her latch was better, my nipples had healed, I had stopped hand-expressing to manage the let down, my hormones had settled and I came out of the fog. It was a nice feeling to know I’ve got this now.
If you’d like to learn how to set yourself up for breastfeeding success make sure to check out my breastfeeding guide. It takes you step by step through antenatal expressing and lots of other wonderful tips and tricks.
If you’d like to connect with Amber you can find her over at Body Birth and Baby
Topics Discussed
Breast Engorgement, Breastfeeding, Postpartum
Episode Sponsor
Medela has worked with generations of mothers to create innovative breast pumps that are practical and intuitive.
Their Freestyle Hands-Free Breast Pump is a game-changer for postpartum because it gives mothers some fantastic options they have not had before. The benefits are impressive. The ultra light-weight collection cups are designed to sit discreetly in-side your bra. There’s no fuss and it’s easy to clean and assemble with 3 dishwasher safe parts. The transparent design makes it easy to align your nipple and ensure the milk is flowing. For a superior hands-free pumping experience, The Freestyle Hands-Free Breast Pump is recommended for its simplicity and ease of use.
Medela blends decades of scientific research with insights from mothers to create practical pumps that lighten the load – quite literally – in early motherhood. Medela – the Science of Care.
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us