Podcasts Amber
EPISODE 391
Amber

“I’m a midwife so I’ve had a birth plan and postpartum plan for ten years. I spent a year really delving into fertility and preconception care; I saw my GP and a naturopath and I did a three-month stint of cutting out alcohol, cutting back on caffeine and taking prenatals and I had a plan for when we would conceive but then I ended up in hospital getting my appendix out. That was my first lesson in having to surrender and let go of control.
“Three months after we started trying we fell pregnant with Winter. I’ve worked in public and private and I truly believe that what’s right for you is different for everyone. I knew birthing at home was not something I felt comfortable with and I didn’t want to go into the city to birth and yet there weren’t many options close to me either. I didn’t want to give birth at my workplace either so I used my parents address and I got access to the MGP programme at a public hospital. I wanted the continuity of care in labour and I also sought out a doula. My husband is also terrified of anything medical so I felt like I really needed extra support to keep him upright, too. I was so happy with my care.
“My pregnancy was really good and to be honest, hyperemesis gravidarum (HG) was my biggest fear. Unfortunately I did have pelvic girdle pain and it started early and was horrendous. Strangely it got better as the pregnancy progressed. I saw my physiotherapist and women’s health physio to assist me with pain and I also did yoga throughout pregnancy to stay as strong and active and manage my pain. I also had pregnancy insomnia so I’d be up at 3am and couldn’t get back to sleep. I made sure that I didn’t check anything in pregnancy; I left that job up to my midwives to consciously take my midwife hat off and be the mum. I was very calm in pregnancy and I think it can go either way for midwives because we see all the worst case scenarios.
“I was so lucky to work in a MGP model for four years and I supported a lot of water births and I loved them so much. That’s why I decided to go to Box Hill because the baths are in the middle of the room and the midwives were so confident in supporting water births and it was something I was really hoping for.
“When my waters broke at 39+2 I moved into mum and dads; thankfully everything was already packed and ready to go. I went into the hospital and they tested my pad and it showed that it was my amniotic fluid, even though it was a little hind leak. I was devastated when it came back positive because I knew I was on the clock so I took oral antibiotics and a plan to check in each day for monitoring. At 3am I woke with a bit of mild cramping but then I went back to sleep and woke up in the morning and there was absolutely no sign of labour. I called my midwife and she encouraged me to come in for monitoring and have a good chat about an induction date. I felt so anxious that day; I just felt out of sorts with all the talk of induction and consent for induction. When I went home my husband and I went for a big walk but regardless, I just didn’t feel good. I woke up again at 2am with a bit of cramping and put a heat pack on and woke up again the next morning still pregnant and not in labour. My midwife brain really kicked in because I think I was scared. I could understand why women make decisions based on fear because I was so fearful and anxious then.
“The next morning I had fresh bleeding and a clot and I knew it wasn’t a show. Birth suite encouraged me to come in and I showed them the photo, the CTG was reassuring and they just encouraged me to go home and the plan was an induction for the next day. Despite feeling anxious I was feeling so reassured so I knew I had to let my anxiety go. My husband and I went out for brunch, we had a beautiful day and ordered dinner…it was just so lovely. Of course, early the next morning I woke up again with cramps and I got up to heat my heat pack and I had a big gush of water and I woke Luke up to tell him. I was really trying to get labour going but nothing I was doing was working so Luke suggested going back to bed and I knew he was right. I think I knew then that an induction was inevitable. I really couldn’t believe that this was happening to me.
“The first step was to confirm if the forewaters had gone and I encouraged the midwife to do a stretch and sweep while she was there. I said to my midwife that I didn’t want to know my dilation and I’m so glad I didn’t know at that stage; I was only 1cm and 1cm long and posterior and for me, that meant my body wasn’t ready. The syntocinon drip went in and it all started.
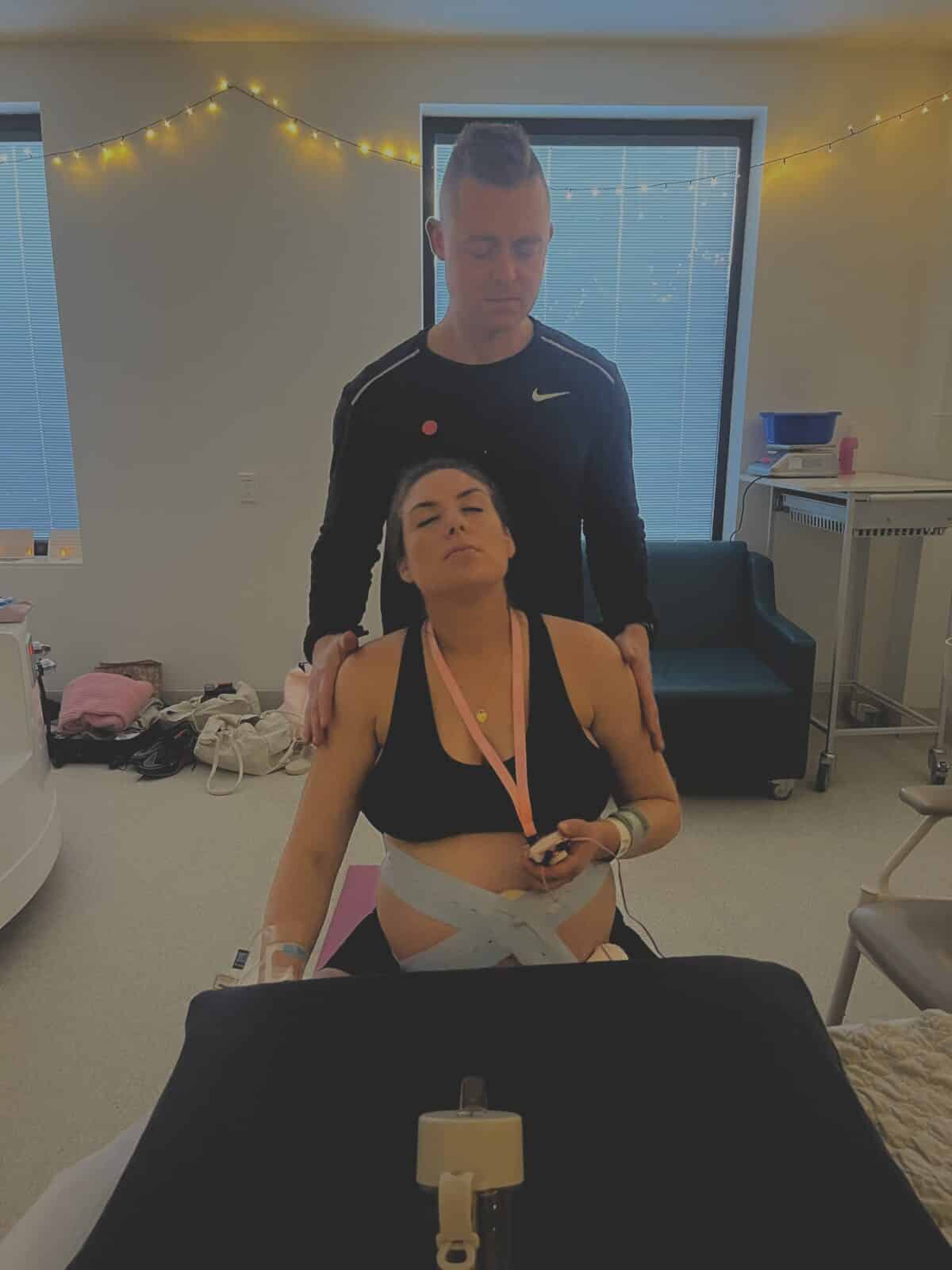
“I had a wireless CTG monitor, there were fairy lights up, affirmations on the wall and my baby’s first outfit laid up. I also had my labour playlist and TENS machine on and within an hour I was having some really good contractions. I had so much trust in my midwife so I didn’t have my midwife brain on at all; I was just taking it one contraction at a time and really resting in between.
“Later in the day I said to the midwife: do you think I should get in the shower? She agreed so I got in there and I was in there for ages. I cried my whole labour; it wasn’t pain or fear but an emotional release. I was so in the zone and so comfortable even though I was in active labour. At one point I felt pressure and felt like I may be in transition and then after a while I realised the pressure wasn’t shifting. I asked for an examination because something didn’t feel right and my midwife told me I was making really good pressure. I asked to know how dilated I was and she told me I was 4 cm and fully effaced but I knew that the urge to push wasn’t good. I tried the gas but I didn’t love it. The midwife that was now on shift was very inexperienced and I didn’t feel safe with her. I went into midwife mode and asked for a new midwife; I couldn’t go to the toilet, I still had a huge amount of pressure and I knew I wanted an epidural. I asked for a catheter to drain my bladder because I was struggling to pass because my baby’s head was so low. That went in and then I asked for another vaginal examination and I had progressed but I was 6cm with a swollen cervix which means I’d been pushing on a cervix that wasn’t dilated.
“I got the epidural but I hated it; one leg was numb and the other wasn’t so I had a lot of hip pain. Eventually it started working and I was so numb and that made me feel so anxious. The fact that I couldn’t move made me feel claustrophobic because I had no physical control. I also knew that it’s hard to come back from a swollen cervix so I was expecting an emergency caesarean at that point. I was still 6cm and swollen so they gave me four hours before they were going to check again and if it was the same, I knew an emergency caesarean would be recommended. At 1:30am I consented to a caesarean because I was still only 6cm and while I can’t remember the times but about 90 minutes later they took me down to theatre and Luke was really struggling with having to go into operating theatre. The anaesthetist topped me up and the consultant told me that as standard practice she’d check how far my baby’s head was down and she told me I was fully dilated. I was so shocked! I said to her: if you need to do high forceps, I would prefer a caesarean. She said the baby’s head was low and she thought I could do it without forceps. She encouraged me to push and I asked for the drape to go down and I put my hand on my uterus and pushed and she told me it was amazing (my women’s health physio had taught me how to push).
“They put the drape back up, gave me an episiotomy and used forceps to help Winter birth. She looked huge! It was my baby and she went on my chest and it was instant love. The birth was nothing like I wanted but I was so in love. I was shifted out of that zone when I heard: has third stage been given? And someone answered: yes. And that’s when I heard the request for 40 units of syntocinon which I knew was postpartum haemorrhage management. She was born at 4:03am and I’d been on syntocinon since 8am the previous day. My uterus had been working so hard for so long, it was a long labour and there was lots of intervention so they and I knew I was high risk for a PPH.
“The obstetrician told me I’d lost 1.8litres of blood within ten minutes which is a large haemorrhage. I was going into recovery and I said to the midwife that I thought I was bleeding. I remember looking at Luke with Winter on his chest and I could tell he was so nervous. The midwife confirmed I was bleeding and she was rubbing my fundus yet every time she let go my uterus wasn’t contracting and blood kept trickling and they’d given me all the medication there was to give. They called a code pink (an obstetric emergency) and even more people came in and they didn’t take their hands off my uterus. I was really fearful of a hysterectomy at that stage. My uterus was losing tone because it had been such a long labour so it was having difficulty staying contracting.
“Thankfully after five minutes the uterus started holding its tone but I was so anxious. I ended up losing 2 litres of blood and they put me on the ward whereas in my hospital, someone with a PPH like that would have gone to the birth suite for one-on-one care. Thankfully Luke wasn’t aware of the severity of it because the staff were all so competent and calm.
“I was desperate for Winter to feed because it helps the uterus contract but she couldn’t latch well so I really utilised my supply of colostrum. I stayed in hospital for one night and then went back to my mum’s house and it was just so nice because I had so much support. Mum was cooking and taking Winter while we slept. We were both shaken from the birth, the midwife came every day that week and we had a really good debrief in hospital and at home. I was able to debrief with my doula and one of my best friends who is also a midwife. Debriefing is essential after a traumatic birth. I looked at every single little part of my labour and I thought: what could I have done differently? What if I had made different decisions along the way and looking back, there was nothing I would have done differently. I just genuinely feel like I did everything I possibly could have; it was just the way it unfolded. That was really healing for me.”

Topics Discussed
Epidural, Forceps, hindwater leak, Induction, MGP, One baby, PPH, swollen cervix
Episode Sponsor
Medela has worked with generations of mothers to create innovative breast pumps that are practical and intuitive.
Their Freestyle Hands-Free Breast Pump is a game-changer for postpartum because it gives mothers some fantastic options they have not had before. The benefits are impressive. The ultra light-weight collection cups are designed to sit discreetly in-side your bra. There’s no fuss and it’s easy to clean and assemble with 3 dishwasher safe parts. The transparent design makes it easy to align your nipple and ensure the milk is flowing. For a superior hands-free pumping experience, The Freestyle Hands-Free Breast Pump is recommended for its simplicity and ease of use.
Medela blends decades of scientific research with insights from mothers to create practical pumps that lighten the load – quite literally – in early motherhood. Medela – the Science of Care.
Categories
Related Products
-
Birth Combs: Harness Your Body’s Natural Pain Relief
$24.95Crafted from smooth, natural wood, our birth combs activate specific pressure points in your hands that trigger your body’s innate pain-relieving responses.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us






