Podcasts Erin
EPISODE 260
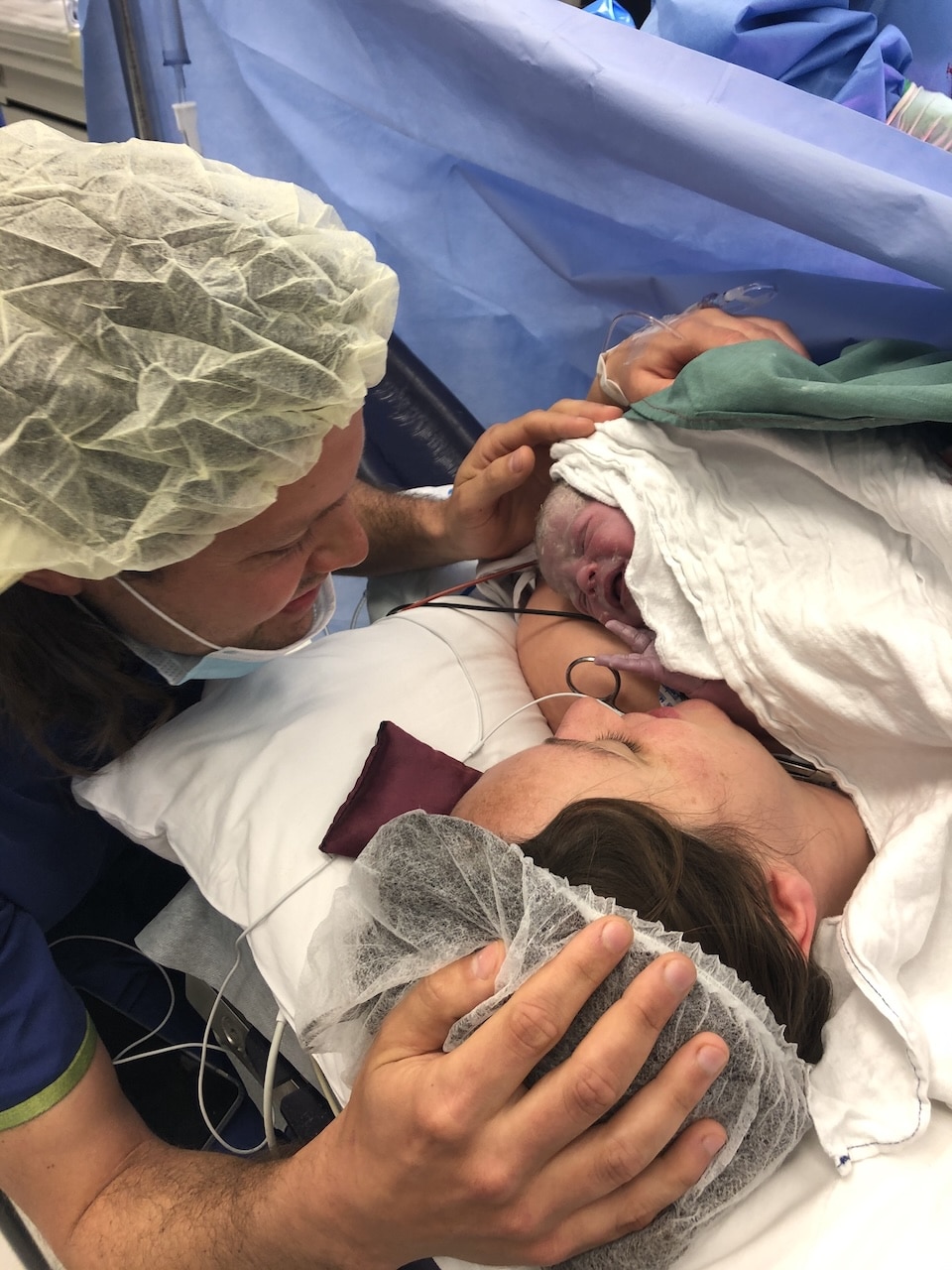
Erin

Erin and her husband Dan live on a farm 90 minutes inland from Canberra. They have a market garden and work hard to supply their local community with fresh produce. They first fell pregnant while living in Canberra and from the beginning, Erin knew the benefits of continuity of care although she didn’t manage to access the midwifery program.
“I chose to do shared care with my GP. We did a calmbirth course and it was the first time I’d considered the physiological side of birth and it really opened my eyes. I didn’t go into the pregnancy with fear, Calmbirth relaxed me and made me feel confident.”
Erin admits that she really enjoyed being pregnant (hence four children) and she’s had straightforward pregnancies which definitely makes things easier. At 34 weeks she switched from GP to hospital care and saw whatever midwife or obstetrician was on staff.
She also saw a student midwife which gave her consistency of care; she attended all of Erin’s appointments and Erin admits it was lovely to have a familiar face at the hospital.
At 37.5 weeks Erin woke up with a lot of bleeding; a lot more than she had been prepared to expect. They went straight to hospital; she wasn’t having contractions and there was no dilation so she stayed for two nights and had a variety of tests and ultrasounds done although she knew all along that baby Toby was fine. She never received a diagnosis but the bleeding definitely eased and then stopped, so she was sent home. Four days later the bleeding started again. At the hospital the CTG showed that Erin was having light contractions and she had started to dilate so she was booked into the birthing suite and a transducer (monitor) was placed on Toby’s scalp as the bleeding was persistent.
“I was 6cm when there was an almighty gush; I passed a huge blood clot and was bleeding a lot. The obstetrician announced that I needed an emergency caesarean. It was really hard because everything had been calm up until that point and then my clothes were ripped off and someone was reading the consent forms to me and the contractions got so much more painful then – it was probably my fear and adrenaline. They started wheeling me down to theatre and as they were trying to put the needle in my spine the pain of the contractions were just intense. The obstetrician came in and he put my legs up in stirrups and he asked if I could push. Toby was there and he was ready to come out but I couldn’t do it, I couldn’t feel anything. Toby was born via forceps delivery and I was really grateful that I birthed him vaginally.
“My placenta had an extra segment, known as a succenturiate lobe but it wasn’t picked up in any of my ultrasounds. It had ruptured, hence the bleeding. The day I went home I had a blood transfusion because I’d lost so much blood in the week prior. We asked a lot of questions moving forward in our next pregnancy when we were considering birthing at home.”
“I found out I was pregnant with Ellie when I was 13 weeks. I was playing sport, running a lot, we had moved to the farm and there was lots of physical activity every day. My cycle hadn’t returned and I was still breastfeeding so I just didn’t think about falling pregnant. We’re an hour-and-a-half from the hospital and because of the bleeding at Toby’s birth I couldn’t access care at the closest hospital, so I had to go to the main hospital in the city. But Toby’s labour was only two-and-a-half hours long so I was concerned about the possibility of birthing on the side of the road.”
Erin did shared care again so she was travelling in and out of the city to attend her appointments; it was difficult, considering Toby was only 22 months. The thought of an unassisted birth on the side of the road was making her really nervous so although she’d booked into Canberra Hospital, Erin started reading and researching about birthing at home. She started having conversations with her family, including her sister-in-law who is an ICU nurse.
At 27 weeks she received a phone call from the hospital to tell Erin that she had been put into the continuity of care program. She met with her midwife who advised her to pack a ‘birth on the side of the road’ bag with a tarp and scissors. Erin refused and went home and booked a home birth midwife, who she met at 30 weeks.
“We had a huge amount of relief once we made the decision and we went ahead with a lot of confidence. My midwife suggested the birth pool and we found one second hand and the only thing that was a worry is that she lived ninety minutes away so we had lots of conversations about when I should call her. There was a good solid birth plan in place so we were feeling really good about it all.
“I was sitting in the sandpit with Toby at 39+3 and I got a surge and then quickly got another one. They weren’t painful but they were coming quickly so I called my midwife and I called Dan who was working in Canberra. I cooked Toby dinner, I was playing with him and went about the evening. Once Dan was home he took over Toby’s care and I was just on all fours in the loungeroom; it was nice to have that space to do what my body needed to do in the comfort of my home. My midwife arrived at 6:15pm and I had been labouring for two-and-a-half hours by then. She was so respectful of my space and she was really hands-off, she just sat there, she didn’t need to do any internals or checks, she just stayed close by and watched what was going on, offering words of support and encouragement when I needed them. When things were getting really hard she said: calm it all down, slow down, you’re not going to birth this baby until Toby is in bed.
“Twenty minutes later I had an uncontrollable urge to push. I didn’t consciously push, Ellie just exploded into the world. It was the most powerful, amazing thing. I’d never felt such immense pride and the feeling of birthing her at home was so wonderful.”
Erin didn’t have a lot of postpartum bleeding and she had a physiological third stage (no syntocinon injection to expel the placenta) and once the placenta was born, she was snuggling on the couch with Ellie who latched so well and fed beautifully. Erin didn’t leave the farm for the first six weeks and once it was time to farewell her midwife, it was a sad goodbye. It wasn’t too long before they saw each other again; Erin fell pregnant with her third, Molly, and started seeing her midwife at 9 weeks.
Towards the end of her pregnancy a strange feeling started creeping in when Erin’s midwife started scheduling her appointments in Canberra, instead of visiting Erin at home. A couple of days before labour, she started experiencing braxton hicks. Her labour began and progressed quite slowly and once the children were in bed, Erin was walking around the
house and swaying and she called the midwife when her contractions were seven minutes apart.
“We laboured quietly in the house, there was a big storm so it was quite beautiful and we had the fire going. Just after 11pm I knew the baby was getting ready to come and I reached down and could feel her head. The midwife was still twenty minutes away and for the first time, in any of my labours, I got really scared. Because that fear creeped in, I stopped breathing and started yelling and she was close but she wasn’t making any progress because I was tensing up. The midwife’s phone dropped out of reception and I felt like I was losing all control. Dan looked at me and said: Erin, stop screaming and start breathing! Three contractions later I squatted in front of the fire and birthed Molly into my own hands. I was in awe of what we had done. Her eyes were open and she was looking at me but she didn’t cry and it dawned on me, I flipped her onto her stomach and rubbed her back and she cried. The midwife arrived but she didn’t take Molly from me for ages, she just let us do our thing.”
Erin’s postpartum care was lacking, Molly was born on December 21st but she didn’t see her midwife again till January 2nd and during that time, Erin had a terrible case of mastitis. She had to initiate phone support and when she did finally visit, she only stayed for seven minutes.
“I wanted to debrief, I wanted help with feeding. That was the only postpartum appointment I had; there were many booked but they were all cancelled. It’s odd because we had a great relationship and I did wonder if I had done anything wrong. I don’t know why I didn’t advocate for myself, or demand my money back; I still think about it.”
There’s just over two-and-a-half years between Molly and Riley but Erin and Dan both felt anxiety about who would care for them during pregnancy and birth. Erin felt like she had to sell herself to two Canberra-based homebirth midwives but they said yes and offered Erin exemplary care. Everything was cruising along until 35 weeks when her primary midwife had a bad accident and could no longer practice. It was an anxious wait to see if a second midwife would come onboard but thankfully it all worked out.
Erin woke early one morning at 39 weeks and went to the toilet to discover a lot of blood. She called her midwife and explained what was happening – light tightenings but nothing productive – and they started making their way to the farm, warning Erin that she would need to be prepared for a hospital transfer.
“As soon as I felt the gush of blood the contractions started hard and fast. My midwife was on her way. It was the shortest and hardest labour. I was making a lot of noise and I don’t know if that was speeding things along but it was definitely intense. The midwives arrived 40 minutes before birth and as the contractions intensified the bleeding eased. They checked Riley’s heart rate and everything was ok so we stayed at home because they knew things were close. My waters broke just before she was born and I felt every part of her be born; I roared her into the world. It was a really primal, intense experience.”
Erin had eight postpartum visits with her midwives which reiterated the power of continuity of care, especially for rural women who have such limited birth options available to them.
Topics Discussed
Continuity of care, Four births, Home birth, Rural and region pregnancy care, Shared care, Student midwife, Succenturiate lobe
Episode Sponsor
Today’s episode is brought to you by BodyICE Woman. BodyICE Woman was created by Olympic Champ and mum of two Lydia Lassila after the birth of her first son in 2011. She realised very quickly from her own experience, a desperate need for ice and heat packs that would help women recover post childbirth and support them throughout breastfeeding. The range includes a Perineum Strip and Breast Pads that can be used as ice or heat packs. When frozen, the perineum strip provides cooling relief to the perineal area which may be irritated, swollen and tender from childbirth. You can also use it to treat Symphysis Pubis Dysfunction (SPD) and haemorrhoids. When heated, the perineum strip can be used during the 2nd stage of labour to soften the perineum and help reduce the occurrence of perineal trauma.
The BodyICE Woman Breast Pads, are designed to fit comfortably inside the bra and around nipples to provide cooling or warming relief from soreness associated with breastfeeding, blocked milk ducts and engorgement. The breast pads also conform around the breast pump and when heated, can help ease the flow of milk and blocked milk ducts.
Made from soft medical grade materials and non-toxic gel beads, the packs remain flexible when frozen or heated, are portable and reusable. They also come with washable sleeves that fit around each pack should you choose to use them. BodyICE Woman is available at bodyice.com, as well as many online and retail stores globally. Follow BodyICE Woman on Instagram for lots of great resources and tips: @bodyicewoman
You can enjoy 30% off BodyICE Woman with the code: AUSBIRTH30
Categories
Related Products
-
The Birth Class
108 reviews$249.00The empowering online childbirth education program that will help you confidently prepare for birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us