Podcasts Rachael Rose
EPISODE 219
Rachael Rose

Rachael fell pregnant very easily with her first baby. She knew that women face challenges throughout the conception, pregnancy, birth and postpartum journey, but she wasn’t quite prepared for the challenge of persistent severe nausea (Hyperemesis Gravidarum HG) that forced her to quit her part time job and take leave from her masters degree. While her partner worked away she spent most days on the couch, eating every half-an-hour to curb the nausea but inevitably vomiting whatever she consumed.
“It was the hardest nine months of my life; we’d only moved to Wollongong six months before, and we were quite isolated. There wasn’t much I could do apart from survive and get through it.
“I had an eating disorder for a decade and mental health issues too. I decided to go with GP shared care and I adored my doctor but she left the practice after my first appointment so I found another GP who wasn’t very helpful and said some things about my weight that really triggered my eating disorder mentality. I managed to find a GP in the end and she supported me through the pregnancy and HG.”
Rachael started to feel better towards the very end of her pregnancy and it was around this time that her caregivers started discussing the possibility of an induction. “My local hospital has a 39% induction rate, there is a culture of induction and their policy is induction at 41+1. Apart from being sick my baby was really healthy so at my 40 week appointment when they said let’s book you in for an induction and I refused, the OB said: Well you’ve got 8 days to fix this problem.”
It was the first of many derogatory comments that she refused to fall prey to. After a few failed stretch and sweeps that left her sore, bleeding and triggered (Rachael is a sexual abuse survivor), she opted to have an induction after 42 weeks but it was when her induction date was rescheduled because of staffing issues that she understood that they’re often not about evidenced based practice but about scheduling and staff availability.
I went in at 8am and had the gel and it worked; by midday I was on the birth unit, doing the work of labour. We did what we could to make the room a really comfortable environment. I was in the shower for hours and hours, my partner was really hands on and my doula was there as a calm and reassuring support. I was getting quite overwhelmed by the sensations; it was all so intense. I was at the bath at one point and my angel midwife came in – she just let me do my thing – it’s kind of birth roulette in the hospital system when you don’t have continuity of care and she said to me: You should have a homebirth next time, don’t bother coming here next time, you’re just doing it all by yourself.
“I refused vaginal examinations 2-3 times, but she continued to ask because she had a hierarchy to adhere to. The fourth time she asked it was 10pm and I finally conceded and I was 4cm. At that time I had that epic crisis of confidence. I requested an epidural and just before the anaesthetist came I started violently vomiting and by that stage I was having rolling contractions and they were so intense.
“From that stage my birth experience changed; the lights were on, I was on the bed, the epidural worked in that it helped me get some rest, I had micro sleeps, I caught my breath but it did slow down my labour so they used syntocinon to augment my labour. They also broke my waters and they discovered meconium staining and the OB was not happy and she said: I don’t know what’s going on with your baby and it would be my suggestion to have a cesarean. And if you do have a vaginal birth, you’ll probably need an instrumental delivery and I only use forceps.
Once she left the room the midwives said: No, you’re going to push your baby out by yourself!
“I pushed for 45 minutes and I birthed her and she was placed on my chest and I felt like the most triumphant warrior woman in the world. I was having to fight, during labour, the outside forces that were trying to change my baby’s birth experience. She was on my chest, we went into our little bubble…they didn’t do any checks for an hour or so. When it was time for me to get stitches the OB invited a registrar in without my consent and said: No one ever tells these women that their vaginas will never be the same again.
“Five hours after birth I was about to transfer to maternity when I had a PPH. This is unfortunately a very traumatic experience for me; I had manual removal of clots, people palpating, medication inserted into my anus. After a triumphant birth I went back to feeling like I had no control. For three years after whenever I thought of my birth I thought of those five minutes. It impacted my breastfeeding initiation because I was so weak. I felt tired and fatigued and I was so emotional – so up and down.”
Rachael’s second pregnancy was a surprise; she was still breastfeeding her three-year-old daughter at the time and experienced severe breastfeeding aversion so decided to wean. She believes that her son chose to come when he did and she was so thankful for mild nausea that eased by 20 weeks.
“Even before I was pregnant I knew that I would have a homebirth, I wanted someone who would love and care for our family during the pregnancy, birth and postpartum. I didn’t have any fear of birth, I saw it as a beautiful rite of passage. I had a backup plan in case I needed to go to the hospital and was well aware of how a PPH would be handled in the home, especially considering I had witnessed one as a doula during my pregnancy. At 38 weeks I signed a memorandum of understanding that outlined that I wouldn’t have an induction of labour and that I knew the risks of going beyond 42 weeks.
“I got to 42+4 with him and it was a mental challenge. I lost my mucus plug at 42+3; it came away throughout the day, I went to the toilet all day and contractions started that night. In the early hours of the night I just laboured by myself; I was crying. I was just so ecstatic that my body was doing it and I’ll cherish those hours for the rest of my life.
“At 3:30 in the morning as soon as my doula, Trudy, walked through the door my contractions stopped and hours later I watched the sun rise and realised I’d been up all night. Trudy woke and wrapped me in a cocoon and I watched Schitt’s Creek. I knew where I needed to go to birth my baby but I was avoiding the pai
n at all costs.
“Trudy came back at midday and then my midwife came, I wailed and sobbed in the birth pool, and considered going to the hospital for an epidural. My birth team knew I didn’t want to be comforted in my discomfort so they held space for me as I journey through labour.
“Trudy convinced me to get on the toilet and in the space between getting out of the pool and sitting on the toilet I transitioned; I was clawing at them, I was begging and I looked at Trudy and I said I didn’t want to do it. She replied: It’s going to be the most painful thing you do in your life and it’s how you’ll meet your baby. I said to myself: Birth is meant to decimate us and this is how I need to be reborn
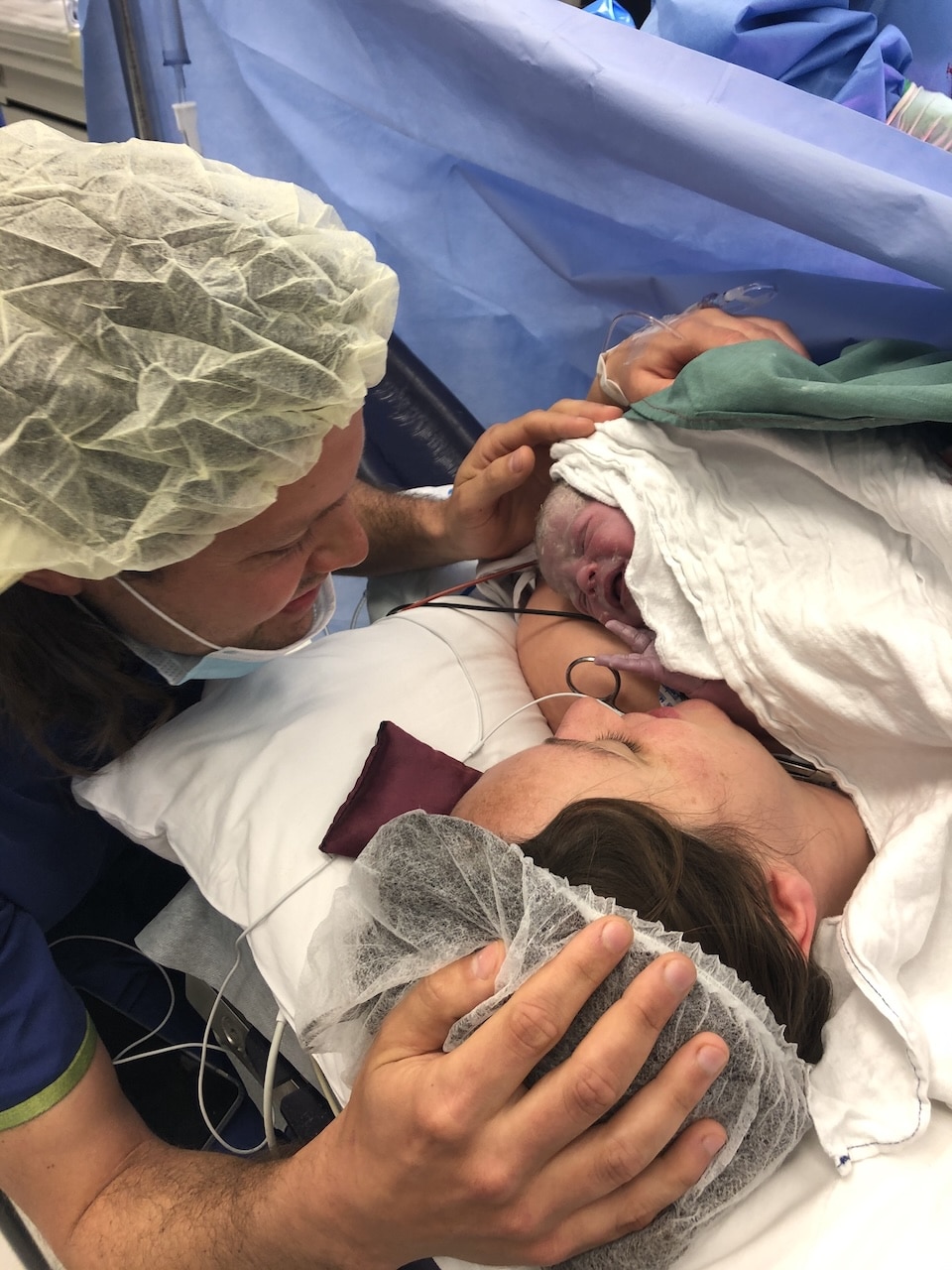
“I started involuntarily bearing down there, I had four contractions and I birthed his head and there was a tsunami of energy pushing down from my head, Tristan stepped in to catch him and I just was in awe.”
Rachael admits that while she won’t be having any more babies, she would give birth all over again if she could.

Image by Serina Crinis

Image by Serina Crinis


Image by Serina Crinis

Image by Serina Crinis
Topics Discussed
Birth rights, Doula, Home birth, Hyperemesis Gravidarum (HG), Postpartum haemorrhage (PPH), Shared care, Two births
Episode Sponsor
Today’s episode is brought to you by Ottie’s Birthday Sale. You can save $10 OFF Discovering Motherhood with the code: MARCH.
You can save $5 OFF my Breastfeeding Guide with the code : MARCH
Categories
Related Products
-
Discovering Motherhood
12 reviews$119.00The 8-part audio program supporting your empowered and confident transition into motherhood.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us