Podcasts 557 | Katie 2 Births, Endometriosis, Inductions, Third-Degree Tear, Brisbane
EPISODE 557
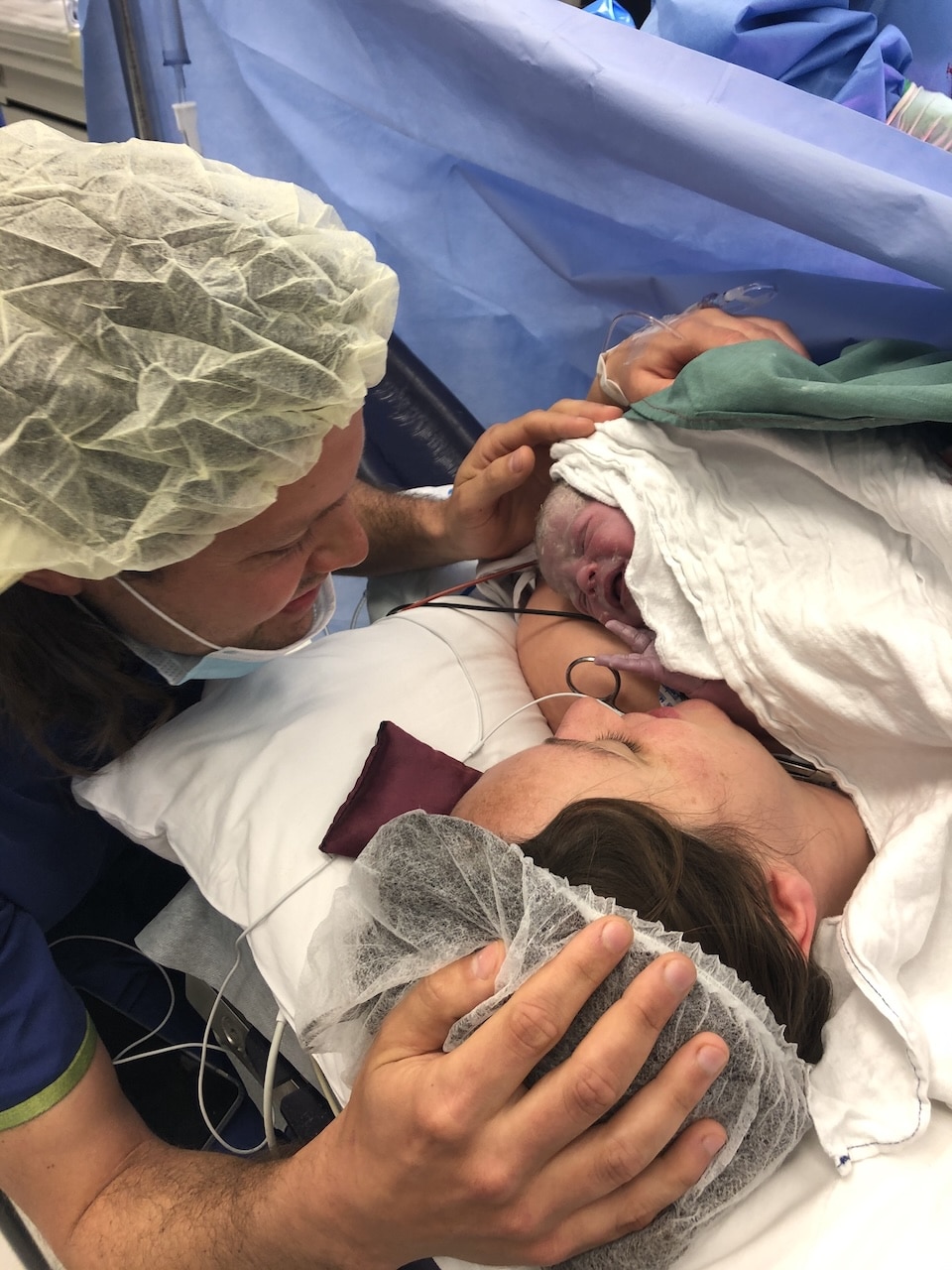
557 | Katie 2 Births, Endometriosis, Inductions, Third-Degree Tear, Brisbane

Three years later, armed with better knowledge and a different care provider, Katie’s second birth was the drug-free, empowering experience she’d always hoped for. She shares invaluable insights about advocating for yourself, the importance of informed consent, and how the right care provider can transform your birth experience. This episode is essential listening for anyone preparing for birth, particularly those with endometriosis or previous birth trauma.
Katie’s story begins with her long journey to an endometriosis diagnosis – a path that will resonate with countless women who’ve been dismissed or misunderstood by healthcare providers. “I started experiencing pelvic pain when I was 15,” Katie explains. “It was never associated with my actual period. I had really bad bloating and pain mid-cycle, around ovulation. When my mum was taking me to the doctor in my teens, they didn’t even discuss endometriosis. It wasn’t even a topic of discussion.”
It wasn’t until Katie was 28 – thirteen years after her symptoms began – that she finally received her diagnosis and life-changing surgery. “I was totally riddled with it all over my bowel, on top of my bladder, not so much my uterus, but on my kidneys as well. Surgery changed my life absolutely.”
Despite her endometriosis diagnosis, Katie was fortunate to conceive quickly. “We started not trying and then we fell pregnant. I think on the second or third cycle we were quite lucky.” Her first pregnancy was relatively straightforward after the initial morning sickness, though she was vigilant about pelvic floor preparation, working with a women’s health physiotherapist who identified that she had a hypertonic pelvic floor.
“I wanted to get assessed because I had a feeling I had a hypertonic pelvic floor and not the other way around, which was true. She said, ‘Don’t do your Kegels. You need to actually learn how to relax.'” Katie also used an EPI-NO device to help prepare her perineum, demonstrating her commitment to birth preparation.
Katie’s first labour began at 41+4 weeks following induction with prostaglandin gel. What followed was an intense, rapid labour that caught everyone off guard. “It went from zero to a hundred. I think I hadn’t even started washing myself when I got a contraction. They just started coming back to back. I think I had maybe a minute, two minutes, and then I had the next contraction.”
The intensity was overwhelming: “I didn’t have time to grab the TENS machine. None of my snacks, nothing. I’d already dilated quite quickly. When I got into the birth suite, I just said, ‘If this is how it started for me, I need the epidural please.'”
Katie’s labour progressed rapidly, but complications arose when she developed a high fever and low blood pressure, causing foetal distress. “Matt made the call pretty quickly to get her out with forceps because she was showing signs of distress. He got her out in one pull, and unfortunately she did need oxygen for about 20 minutes.”
What Katie didn’t realise at the time was the extent of her injury. “I knew I had torn significantly, but the actual degree of tearing wasn’t actually mentioned.” It wasn’t until her second pregnancy that she learned the full truth: “Brad was the one that told me the level of tearing. I had a third-degree tear.”
This lack of informed consent is unfortunately common, and Katie’s experience highlights the importance of asking questions and understanding your medical records. The recovery was challenging, complicated by burst stitches and infection, yet Katie remained positive about her overall experience.
Preparing for Baby Number Two
When Katie’s local private hospital closed its maternity ward, she had to find new care. This led her to Dr Brad Robinson at Greenslopes Private Hospital – a decision that would transform her birth experience. “The difference with my second experience with Brad is he explains everything in great detail and gives you all of the options. It’s very clear that it’s your decision, but he needs to make sure that you’re fully aware of the pros and the cons of each.”
Brad’s thorough approach included reviewing Katie’s previous birth notes and arranging an endoanal ultrasound to assess the healing from her previous tear. “Thankfully everything was really intact down there. I had no issues. There was no trauma to the tissue, and Matt had done a really good job at stitching me up.”
Given that Katie’s second baby was tracking larger than her first, Brad discussed the risks and benefits of induction versus waiting for spontaneous labour. “If I was to deliver vaginally and have an injury just as bad or worse, I probably wouldn’t be as lucky with the outcome,” Katie reflects.
The decision to induce at 40 weeks was made collaboratively, with Katie feeling fully informed and supported. “I was adamant that I wanted to deliver vaginally. I think I had listened to stories on your podcast – I know it can be done, and I am fully aware of the risks.”
Katie’s second labour was everything she’d hoped for. Starting with just a small dose of prostaglandin gel, her body responded beautifully. “I started cramping pretty much straight away. I put the TENS machine on at about 11pm. I just rested with that TENS machine on super low but really regular cramping.”
The atmosphere was completely different this time: “I put on our wedding playlist. We ended up having old school bangers and R&B music playing. Between contractions, I was having a bit of a boogie. It was a really fun labour, to be honest.”
Katie’s description of her drug-free labour is inspiring: “The TENS honestly was giving me so much relief. My contractions stayed really steady at two to three minutes apart the entire time. The only position that felt comfortable for me was standing, swaying and bent over the bed.”
When it came time to push, Katie faced another challenge – Archie was born with his hand by his face. “Right at the last second, Archie stuck his hand up by his face. He ended up birthing his head and his hand at the same time.” Despite this complication, Katie achieved her goal of an intact perineum, suffering only a second-degree tear due to the hand presentation.
“Brad said I probably wouldn’t have torn at all if it wasn’t for the hand,” Katie notes, highlighting how sometimes complications are simply unavoidable, regardless of preparation.
The difference in recovery between Katie’s two births was remarkable. “Honestly, night and day. I think having the drug-free birth – physically I felt really good this time round. The healing with my stitches and everything was so much faster.”
Katie’s honest account of both triumph and trauma in birth provides hope and practical wisdom for mothers navigating their own birth journeys. Her story reminds us that while we can’t control everything about birth, we can control how we prepare, who we choose to support us, and how we advocate for ourselves throughout the process.
Episode Sponsor
Support for Your Fourth Trimester and Beyond – with iL Tutto
Your nursery chair matters – you’ll spend countless hours feeding, cuddling and soothing your baby. iL Tutto’s Nursing Chairs support real parenting moments in absolute comfort.
Choose from Electric Recliners and Recliner Gliders, ergonomically designed with whisper-quiet recline and built-in USB charging. Beautiful, practical fabrics include plush Teddy-Fleece and new Latte woven fabric.
Exclusive offer: Use code RECLINER20 for 20% off at iltutto.com.au
Ends 31st July 2025.
iL Tutto. Designed for parents. Loved by babies.
Categories
Related Products
-
The Birth Class
108 reviews$249.00The empowering online childbirth education program that will help you confidently prepare for birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us