Podcasts Katie – plus-size pregnancy, doula, induction, vaginal birth, PPH
EPISODE 478
Katie – plus-size pregnancy, doula, induction, vaginal birth, PPH

“As someone who is entrenched in the media landscape especially around plus-size bodies, I was aware of the fertility challenges that can exist when you’re plus-sized and the limited options to access fertility treatment if needed. Brendan, my husband, and I just decided to start trying. I’d been off birth control for six-to-eight months because it didn’t work well with my anti-depressant. I had a regular cycle and I was aware of my fertile windows so we started trying and I conceived in that first month.
“Like most plus-sized women, I was shoved very assertively into a very medicalised model of care. I went to my GP early and had a dating scan at 7 weeks and was referred to my local public hospital at 10 weeks. When the midwife phoned for my intake I requested MGP care because I’d heard such good things about it and my goal was a low-intervention, physiological birth and I was told straight away that I wasn’t eligible because of my weight. It was only when I attended my first appointment at the hospital I was informed that I was labelled as high-risk because of my high BMI. Once you’ve been told your pregnancy is high-risk; it sits in your brain. I had extra appointments and the conversational tenor is that they’re looking for something that’s wrong. I had to do the early gestational diabetes test at 16 weeks and then again at 26 weeks and both came back negative.
“I wasn’t confident that I’d have the birth I wanted; I felt like I was going to be pushed into a medical birth. By the time I was 20 weeks, I hadn’t seen the same person twice. I didn’t know if I would see a midwife or OB, or what tests I’d need and what the test results would mean. I was weighed a couple of times and I refused a few times. They requested towards the end because it would inform anaesthetic requirements.
“At 24 weeks I had an appointment with an obstetrician and it was the only negative experience I had. She told me that because of my BMI I’d need to be induced because the risk of stillbirth escalated for someone like me after 38 weeks. I read Sara Wickam’s book ‘plus-sized pregnancy’ and I knew the stillbirth risk was still very low and I felt confident enough in my background in advocacy to ask her if the caesarean rate was 50 percent for plus-sized women because people with high BMIs are pushed into medicalised streams of care or is there a physiological reason. I left that appointment feeling quite distraught because I felt railroaded into what my birth would be like and the kind of care I would receive.
“I decided to get a doula to help support me. We clicked straightaway; she’s kind and gentle but I could tell she was steely and she is also a registered nurse so she was able to bring that medical understanding with her. She helped me realise that I wanted to feel like I was consulted and to give consent every step of the way, regardless of what intervention I did or didn’t have. I didn’t have any fear of birth and I think it’s because I had knowledge and I felt informed so I started to feel much more empowered and in control.
“In my third trimester I saw two different midwives and didn’t have to see another obstetrician after my negative experience. I was told very early in my pregnancy that I wouldn’t be able to access waterbirth at the hospital and that’s because the mechanical sling that gets you out is only rated to 130 kg but I just wonder if maybe they should focus on getting better equipment. In the high risk programme I met with an anaesthetist and they spoke to me about the fact that the placement of an epidural can take a bit longer and that if I did want one, it could take over an hour for it to kick in. I was also asked, pretty regularly, from 32 weeks how far I wanted to go because they wanted me to be induced.
“Apart from pelvic girdle pain, it was a very normal pregnancy. I was halfways through my 38th week when I was starting to experience lower back pain and abdominal discomfort but it was nothing regular and I was just monitoring it with heatpacks and hot showers. My face, feet and hands were quite swollen and I mentioned all of this at my 39 week appointment which I had with the obstetrician I didn’t like. I mentioned the pain, the swelling and she kind of dismissed it as late pregnancy symptoms. I did a urine test – which I’d done throughout pregnancy and didn’t know they were looking for protein in the urine as a sign of preeclampsia. She did a stretch and sweep and she said my cervix was soft but still closed.
“I went home and I was in a lot of pain and while everyone was telling me it was normal, I couldn’t get my head around. My doula encouraged me to call the hospital and they welcomed me in and they did the CTG which I found very tedious because of my anatomy and when the doctor came in she told me they were a bit worried because my blood pressure wasn’t high but it’s been low all pregnancy and more concerningly was my blood tests showed my platelets had halved and that paired with the swelling meant they weren’t inclined to send me home. They wanted to keep me overnight to monitor because it wasn’t a good combination of things and were all signs of pre pre-eclampsia. I was also Group-B strep positive so I was aware I would need to go on antibiotics once my waters broke.
“I stayed that night and the next morning the doctor strongly suggested an induction. The midwife took the time to tell us what the process would look like, what it would mean for my labour and she answered all our questions and then I called my doula to debrief and I got to the point where it really did feel like the best option. At 4 pm they did the balloon catheter and I was already 1cm dilated so things were definitely ready. It was uncomfortable and it prompted contractions which were coming every 40 seconds so they gave me morphine which helped me sleep overnight.
“They moved me to the birthing suite the next morning and broke my waters about 8:30 am. I had agreed to a foetal scalp monitor because my pain relief of choice – remifentanil – which is patient. It’s administered by an anaesthetist through a drip. The big appeal to me is that it’s patient-administered and it’s described as fast-acting and fast-dissipating; you have to be in tune with your contractions because if you miss it, you miss the pain window. I loved that I could stay active with it and Brendan remarked that I seemed more like myself when I was on it. I knew I was going to need a cannula for the Group-B strep antibiotics so I could have the remifentanil through the same cannula anyway.
“At about 11:30am I got a vaginal examination and I hadn’t dilated that much and I really could see how I could keep going. Everyone was telling me it was all normal and I turned to my doula and told her then that I thought I would need an epidural. She told me that she’d heard me but she encouraged me to keep going and that was when I went from using the gas to the remifentanil. I felt really comfortable on the bed but I was cold because of the remifentanil so I had blankets on me. They had to check me again at 2pm and I was 9 cm and at that point it was getting really intense; my contractions were coming hard and fast.
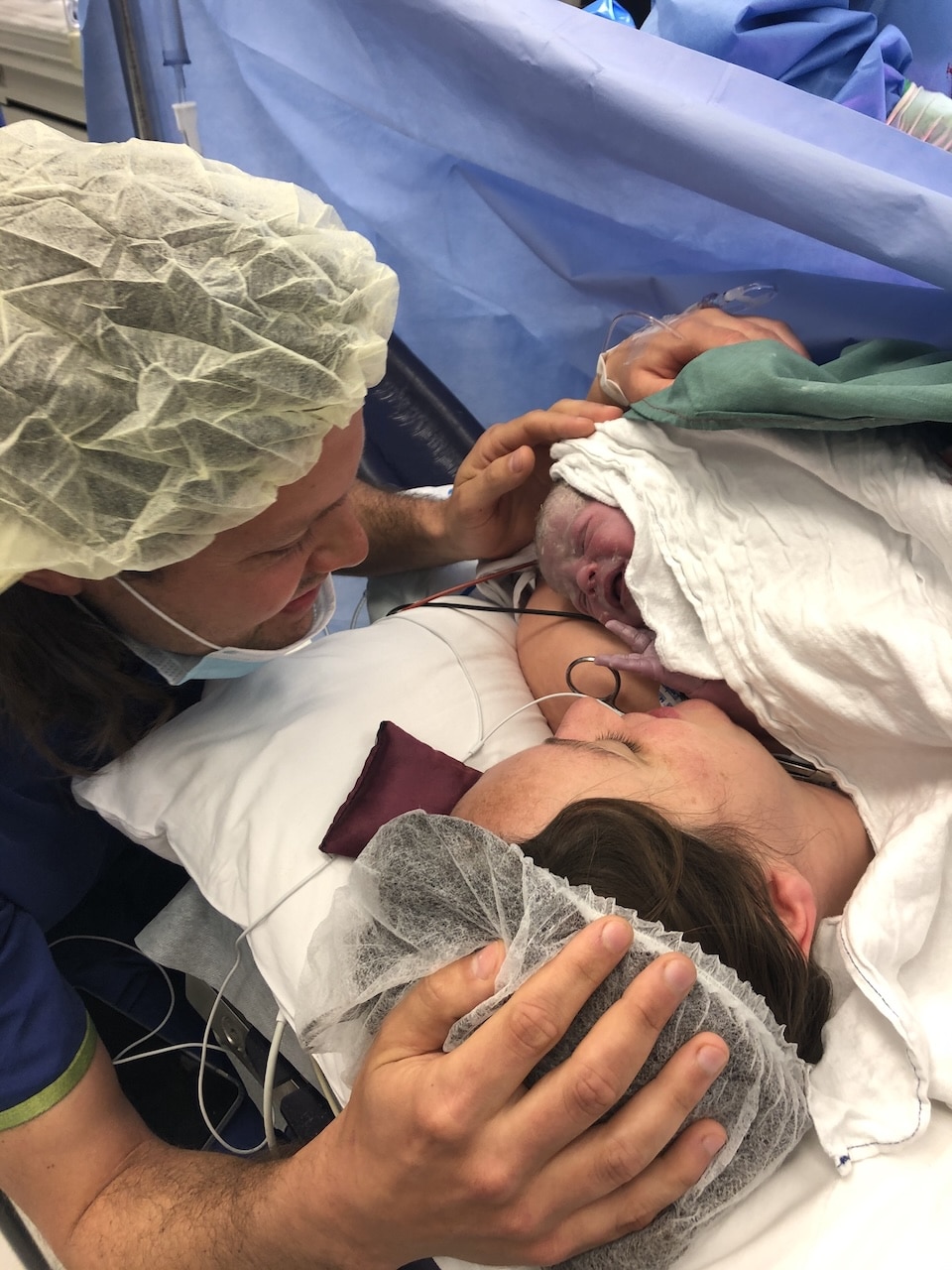
“At 3pm I sat up in the bed and dropped my legs down and I pushed for 25 minus and my baby was born. She was crying and beautiful. I birthed the placenta and told me I needed a few stitches and my doula warned me that it would be uncomfortable and painful. I couldn’t help but notice that more people kept coming into the room and they started mentioning that I’d need another cannula put in as I was having a postpartum haemorrhage.”
Katie loved the book Plus Size Pregnancy by Dr Sarah Wickham


Topics Discussed
Doula, Induction, One baby, plus-size, PPH, Vaginal birth
Episode Sponsor
Today’s episode of the show is proudly brought to you by Once Upon. You all know how much I love making our photo books and prints on the Once Upon app and guess what, you can create your book today and save 25%. Just use the code books25 at checkout.
This offer is valid from May 26th until end of day on June 2nd 2024. Head to Once Upon.
Categories
Related Products
-
Birth Combs: Harness Your Body’s Natural Pain Relief
$24.95Crafted from smooth, natural wood, our birth combs activate specific pressure points in your hands that trigger your body’s innate pain-relieving responses.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us