Podcasts Jo – Placenta previa and VBAC
EPISODE 398
Jo – Placenta previa and VBAC

“We were trying to conceive for six months and then I decided to seek some professional advice. After I’d done a few tests I was referred to an OB/GYN and she told us that everything looked normal. I did tubal flushing and of all the things I’ve experienced it was the most painful. I was awake and they gave me panadol but that didn’t cut it. It’s quick but it’s very uncomfortable; they use a balloon to dilate the cervix and then flush the tubes. The first attempt to conceive after flushing increases your chances but it didn’t work for us. After that we saw a fertility specialist and that was at the one year mark.
“I was diagnosed with unexplained infertility at that point which was a frustrating diagnosis; I wanted to know what was wrong so I could fix it. This was at the start of covid so I had to go to all the appointments on my own. We went straight to IVF; our doctor told me I was ovulating perfectly and since we’d been trying for a year, the chances of succeeding with IUI was low. At that stage our relationship was really challenged. We got 20 eggs and 5 embryos from the first round and we were so lucky; we conceived Isabelle on the first transfer.
“I chose a private obstetrician from the women’s obstetrics and gynaecology team and loved that model of care. I felt completely normal in pregnancy and I had so many scans because I was just convinced the baby wasn’t there. It was only after the 20 weeks scan and shortly after when I started showing that I really relaxed into the experience.
“At that scan it was noted that I had placenta previa and the obstetrician who was doing the scan said it was very unlikely that the placenta would move from where it was because it was completely blocking the cervix. My obstetrician reassured me and definitely didn’t catastrophize it; she never made me feel unsafe. I was really looking forward to birthing vaginally so I grieved the loss of that experience at 20 weeks and from then on I didn’t do any birth preparation because I didn’t want to make myself feel bad.
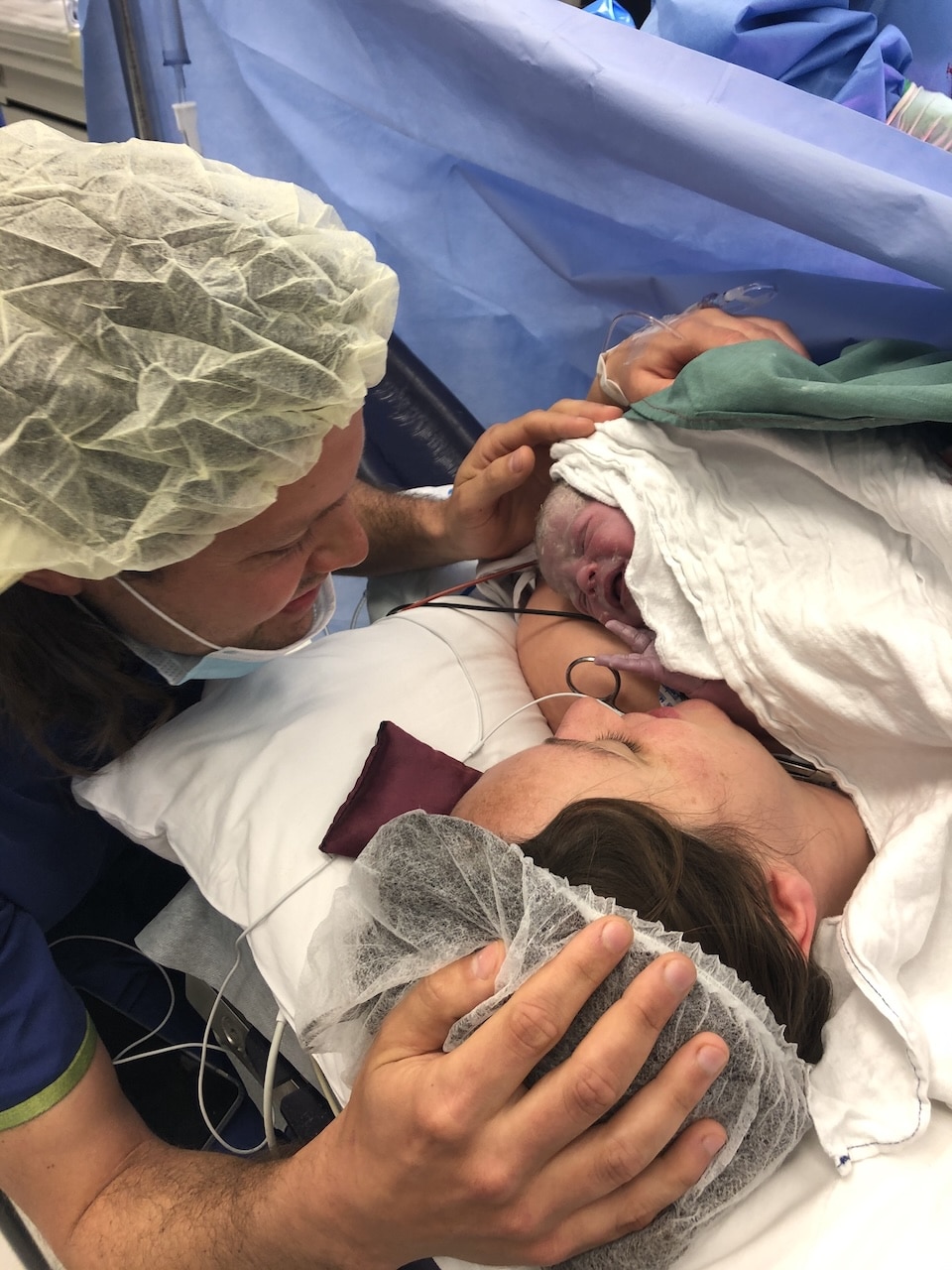
“My caesarean was planned for 38 weeks on the dot because if I had gone into labour, it would have been very high risk. I was booked in for 4pm so we went out for breakfast and I got a blowdry. It was so strange though, very surreal. I was a bit anxious because I didn’t like the idea of an epidural and being numb. I could feel the pressure and the bed moving but she was out really quickly and was crying immediately and has been a firecracker since. We had our first breastfeed in recovery but then I had a haemorrhage. They managed me in recovery and got it under control with medication and fundal massage.
“I stayed for four nights and we were ready to go home by then. It was great to establish my breastfeeding while I was there and I was determined to breastfeed so I used the lactation room. I expressed colostrum in pregnancy which was great because the colostrum took the edge off when she woke up ravenous and then I would continue feeding her.
“I felt like someone had handed me a baby that wasn’t my own. It’s hard to admit to that because people talk about this big rush of love and that certainly didn’t happen to me. In pregnancy I was screened for postnatal depression and my obstetrician suggested I sign up to the emails from COPE and I got an email every week during pregnancy and first 12 weeks postnatally and they explained what’s normal and what’s not. They explained that it wouldn’t necessarily be immediate love like the movies. I knew I was going to look after her but it was a slow burn, learning to love her.
“We moved to Geelong when Bella was 18 months old. We went back to the fertility expert when Bella was one and she encouraged us to try conceiving naturally before we transferred an embryo. She suggested ovulation tracking with scans so we knew exactly when to try. We fell on that first try but I miscarried at 8 weeks. It wasn’t right from the start; everything didn’t look quite right from the start. I miscarried at home; it took about 24 hours to pass and then it was like a heavy period.
“The fertility specialist said the chances of falling pregnant are highest the month after miscarriage and she was right, we fell pregnant straight away. I was more apprehensive but I’m a numbers person, so I relaxed into it a bit more. This pregnancy was so different; from the moment I peed on the stick I was nauseous. It was a very uncomfortable pregnancy.
“I considered going back to Frances Perry House but an obstetrician in Geelong was recommended to me and she was lovely. I met her at 8 weeks and one of the first things she suggested was a VBAC. I burst into tears because I was so shocked at how supportive she was. She wasn’t saying I had to do it, but she gave me options. I was so pleasantly surprised.
“I went home to my husband and talked to him and at that stage I felt like it was too risky. I thought I’d have a repeat caesarean. But then I started doing the research and my OB told me I was a great candidate for a VBAC. The numbers started to feel more comfortable as time went on. At about 20 weeks I started to feel more comfortable with the stats.
“There was some uncertainty with the hospital; it closed its maternity ward and that took over a lot of my headspace. At that stage – about 30 weeks – I went back to my plans to have a caesarean because there was so much unknown. I received a phone call from the hospital to say that they were closing. They said it might be open, it might not, but they were letting me know so I could make an informed decision and then I asked for my options. They said it was up to my obstetrician to find another hospital or I needed to change obstetricians.
“My obstetrician was amazing and she acted on it so quickly and arranged for me to birth at the other private hospital. I felt confident attempting a VBAC; the midwives at the new hospital were so supportive and made me feel really safe.
“I had really bad varicose veins in my legs and vulva; I wore compression tights from my feet to my belly. It was a feat to get them on in the middle of summer. They helped but they were so uncomfortable. I had to go on clexane and aspirin because the veins started clotting but I had to come off them at 38 weeks. My obstetrician said the veins wouldn’t prevent me from having a vaginal birth because I was very considered; they were on my labia and internally in my vagina too.
“I didn’t want to go over 40 weeks so I tried all the things to kickstart labour; sex, raspberry leaf tea, curb walking around the streets of Geelong. I also got acupuncture and they attached electrodes and it was like a supercharge; I went into labour that night. I’d had spurious labour for weeks but that night I woke at 2am with cramps I couldn’t sleep through.
“I went into the hospital at about 6am for monitoring and they confirmed the baby was happy and they encouraged me to go home. I actually went to a Mother’s lunch but by dessert I needed to go home. We went back to hospital and they were really busy; their birth suites were full so my obstetrician came and checked me; I was fully effaced at 4cm by that point and she encouraged me to go back home for a few more hours to get things progressing.
“I was getting more uncomfortable and by 7pm I really felt like I needed to be in hospital. I had a beautiful midwife and I chatted with her; I was so relaxed. I had chatted to my obstetrician about not labouring for too long and she’d never put a timeframe on it but by this stage I had been labouring for 24 hours. That’s when she decided to break my waters and the pain went from zero to a hundred. I was 6 cm at that point but I progressed really quickly then.
“I was using the TENS machine which was great. I felt the urge to push about three hours later and I asked the midwife to get the obstetrician. I started pushing but she wanted to check me and she confirmed I was fully dilated. After a while I told her that something wasn’t right so she had a decent look and I had a cervical lip so she told me I needed to stop pushing. She suggested an epidural because I said I couldn’t stop pushing. The anaesthetist was amazing and I rested for an hour and then I was ready to push.
“I was in stirrups and she told me how to push; she outlined what needed to happen and how long I could push for because she was mindful of my long labour. I really appreciated that because I knew what was to come and I’d given her consent to use a vacuum if necessary. I started pushing and within about 15 minutes my labia swelled so quickly that she said I could only push for a short time more. I had an episiotomy and vacuum and Albert was born soon after. His head and shoulders were born and then the obstetrician encouraged me to grab him and I pulled him up.
“I was losing quite a bit of blood at that point but she thought it was from the varicose veins. I lost 1.1litres so it wasn’t huge but it was substantial. I felt okay and it was all managed in the birth suite. The swelling went down pretty quickly. The episiotomy was uncomfortable but I just used pain relief and ice packs. The vulva varicose veins were gone within a few days and the veins in my legs have gone down; they’re just cosmetic now. I walked out of the birth suite which I was fascinated by; so different to a caesarean. The recovery has been so much better than a caesarean.”



Topics Discussed
IVF, Miscarriage, Placenta previa, Planned caesarean, Private obstetrician, Two Babies, Unexplained infertility, Vacuum, VBAC, vulva varicosities
Episode Sponsor
Our friends at iL Tutto offer the widest range of Nursery Chairs, designed here in Australia. Their range includes the traditional rocking chair, Glider and Recliner chairs, even the hugely popular Electric Recliner Chairs, in a mix of premium, Standard 100 by OEKO-TEX® certified fabrics in an array of trending colours from white, to various shades of creams and greys, all of which are easy to clean and maintain.
Now for the exciting news…. iL Tutto has an exclusive secret to share with our listeners!
Starting this Friday 23rd of June, iL Tutto will start their end of financial year sale, with huge savings across their Nursery Chair range, up to 30% off! You can expect to see their gorgeous Paige Glider & Recliner in Bouclé Nursery Chair with a saving of $269!… its stylish frame will complement any room in your house, meaning it can live on beyond the baby years.
iL Tutto is also providing the Australian Birth Stories audience an additional discount on top of the 30%! Use code ‘extra5’ at checkout for additional 5% off, that’s up to 35% off storewide.
Shop now at iltutto.com.au, sale starts Friday 23 June and ends at 11:59pm Sunday 02 July. See their terms and conditions page for more details.
Categories
Related Products
-
Birth Combs: Harness Your Body’s Natural Pain Relief
$24.95Crafted from smooth, natural wood, our birth combs activate specific pressure points in your hands that trigger your body’s innate pain-relieving responses.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us