Podcasts Paige
EPISODE 337
Paige

Despite the fact that she was trying to conceive, Paige and her partner Patrick were still shocked when she found out she was pregnant. As a nurse and midwife she knew she wanted to be in the MGP program so she went to her GP early to get a referral but unfortunately she didn’t get in.
“I went to see a different GP because mine was away and I walked out of that appointment thinking if I didn’t know anything about pregnancy, I would have come away with no information and a lot of overwhelm. My partner couldn’t come to my scans but I managed to do my scans with people I knew through work which was nice. As a nurse and midwife I was definitely overthinking things and I found myself having to switch off my professional brain.
“I went into my birth a little naive; I’d seen so many women give birth and all the births I’d witnessed as a student were really positive. I knew I could do it but I think I was overly confident. I went to 41+2 and I went to my 41 week appointment and I admitted that Scarlett was moving a bit less than normal. I was sent straight for an ultrasound and that showed that she had no amniotic fluid left around her – known as oligohydramnios – and they think that’s just because I was overdue.
“I was a bit panicked but it was nice knowing that my midwife, Sophie, was there. She encouraged me to go home, have a shower, pack my bags and come back in at night for a balloon catheter induction. I felt really good about the catheter because there were no hormones involved. I didn’t find it painful thankfully; I just lay there watching tv in the postnatal ward and enjoying the time before labour. Unfortunately it stayed put all night and then I was moved to the delivery suite at 7am and they broke my waters but because there was so little amniotic fluid nothing came out. They hooked me up to the syntocinon drip and the contractions came on really hard and fast. I accepted the fetal scalp monitor because I knew monitoring was important but I also wanted to be free to move. I was in the shower when I felt like I was losing control, I felt really overwhelmed and I was crying. In between my tears I was being asked to get on the bed because Scarlet’s heart rate was dropping and at that point I was glad I had the fetal scalp monitor because I knew it was accurate. The midwife pressed the call bell and everyone came rushing in. I knew Scarlett may have been laying on her cord so I changed position because I knew that can often bring the heart rate back up. I had a vaginal examination and I was 3-4cm so they gave me an injection to slow the contractions and because her heart rate had stayed down for 10 minutes they called a code green emergency caesarean. I had no pain relief on board so they suggested a general anaesthetic. I was just crying when they said that…I wanted to see my baby being born, I didn’t want to be asleep.
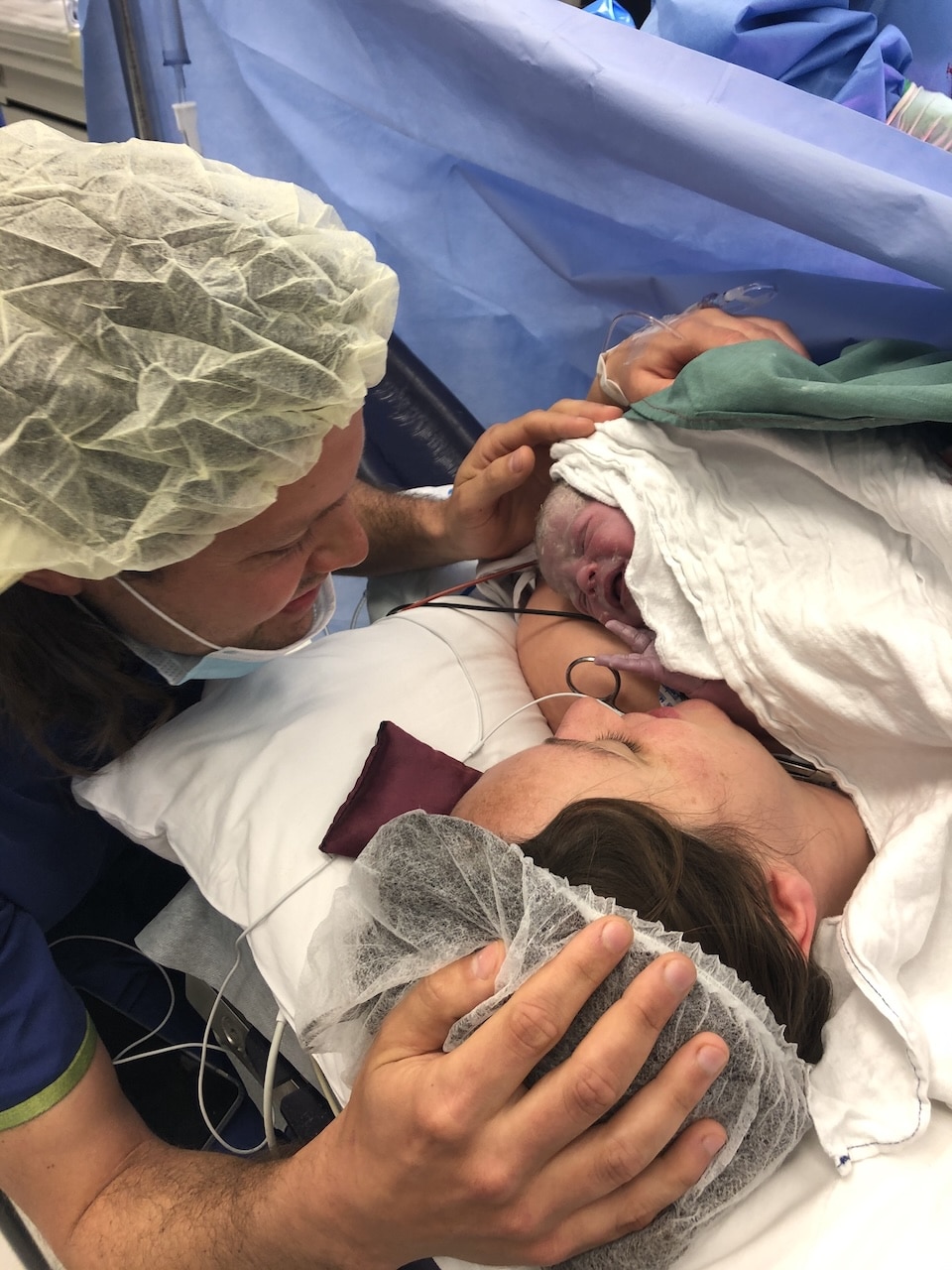
“Sophie my midwife, noticed that Scarlett’s heart rate had come up and she suggested a spinal instead of the general. The anaesthetist agreed so they took me in for that and then they brought Pat in. It was quite traumatic for me so I can’t really remember anything from my time in theatre. We have a very cute video which I’m so grateful for; one of the midwives took it and it’s so special.
“Scarlett breastfed straightaway in recovery. I went home at 2pm the next day and my mum was going to be there so I knew I was going to be well looked after. Sophie came to my house so that continuity of care was beautiful. Five days after Scarlet was born I woke up at 5am to feed her and filled a pad and then I sat on the toilet and it was like a tap, just blood coming out. I called an ambulance and they took me with lights and sirens back to the hospital.
“Clots had formed in my cervix and I was diagnosed with cervical shock, which is where your cervix isn’t able to clamp down. I was moaning like I was in labour again. Finally they retrieved clots, I was given morphine for the pain and they spoke about taking me up to theatre for a D+C. I remember a midwife brought me a pump, she had lip balm for me and helped me pump before I went to theatre. Pat then took the milk home for Scarlet.
“I woke up in the postnatal ward and the first thing I asked was what happened? I had a D+C to clear everything out and I had IV antibiotics for 24 hours and an iron infusion and then went home to resume my postpartum. At six weeks Pat broke down, he felt like it was all a bit much, the weight of responsibility and the trauma of me going back to hospital. I got my mum to come over and we set up a bed for him in the spare room and he had a solid night’s sleep and then he saw a psychologist because he had postnatal depression in those first few weeks.
“I pushed my feelings down until I was pregnant with Violet. I had a lot of trauma and flashbacks of sitting on the toilet bleeding. I was referred to a new hospital because we’d moved and because I’d had a previous caesarean I was told I needed to see an obstetrician and because it was covid I wasn’t able to bring Scarlett with me. I opted for shared care with a GP who was also an obstetrician which was a more family friendly option for me.
“When people around me started to have positive vaginal births, I was so happy for them but so disappointed that I didn’t get that experience. I was just so sad. I booked a birth debrief with Rhea Dempsey and it went for about two hours. She’s amazing, it was so good. Rhea just wanted to hear it from my point of view and jumped in every now and then to ask good questions. This helped me work out where my sadness, trauma or grief was coming from. The trauma for me was feeling out of control, not in control of my pathway, more like a passenger than an active participant in my birth. For Violet’s birth I wanted to be in control and labour and birth actively.
“I contacted Bree who is a doula and she’s amazing. She’s had an emergency caesarean, she’d attempted a VBAC and had another caesraean and then she eventually got a VBAC and because of her experience, I felt like she had lived experience in all the possible birth outcomes for me. Frankston Hospital were so supportive of me planning a VBAC and happy for me to go to 42 weeks for that.
“I was getting really intense braxton hicks at 37 weeks and they were quite painful but very on and off. The day after Scarlet’s birthday – I was 37+4 – I had a big cramp and then my waters broke. I called Bree, I didn’t have a bag packed and I didn’t have my birth preferences printed. My plan was to avoid the hospital as long as I could, the waters were clear and I could feel Violet moving and I told the hospital I was happy at home and I would come in the next morning for monitoring if I wasn’t in labour and they were happy with that.
“As soon as Scarlett went to bed I started contracing but Violet was posterior and the contractions were on and off and they stopped by the morning. I went in for monitoring and the midwives were supportive of me to go home and wait for labour to start, as long as I went in at 4pm and then 8am for monitoring and to check that I didn’t have a temperature. I had a big contraction every ten to fifteen minutes all day until we went back in at 4pm. Violet was so happy on all the monitoring and then I laboured overnight at home again and went in to hospital for monitoring again. I spoke to the obstetricians and they were happy for me to go home and try and go into labout and agreed to return the next morning for an induction if I didn’t go into labour.
“Bree came over with her doula bag, we walked in the rain, I did nipple stimulation and then by midnight I knew I’d done everything I could do and was happy to have an induction the next morning. I burst into tears as soon as I got into the room, all the fear from my last birth came back. My midwife was so lovely and went really slowly with everything and helped me get in the zone.
“I had asked for a half dose of syntocinon in my birth plan and I didn’t want them to put it at full capacity and I wanted it to increase really slowly. I put my music on, I sat on my ball and I started to get nice contractions. Violet was still posterior but I was having more contractions and they were lasting for longer. I listened to my playlist and got in my zone. I accepted vaginal examinations but I told them I didn’t want to know. I laboured nicely till 6pm and had another examination and apparently I was 4cm then. When it got dark my contractions got quite close together and I got quite distressed. I wanted the epidural but I opted for the gas instead and I got quite cranky and unreasonable and that’s when Pat and the midwife thought I was transitioning. Clare, my doula, and Pat tried to bring me back to centre but the midwife agreed to get me the epidural. The anaesthetist was ages away and then when I sat up on the side of the bed for the epidural and started making a lot of noise and the midwife asked if I was pushing. I got the epidural and Violet coped really well with it, that was about 9:30pm. At 10pm they did a cervical check and I was 10cm.
“I had two hours to rest which was plenty of time for her to descend and then the epidural had worn off a lot which meant I could feel the contractions. I pushed for under half an hour and there was a mirror so I could see her head coming down; it was so surreal. The pressure of her head crowning was so intense, I breathed her head out and the rest of her body came out and I grabbed her and brought her up to my chest. Pat and I were both crying, it was the moment we didn’t get the first time. I was just so over the moon that I’d got my VBAC.”


Topics Discussed
Birth trauma, Doula, Epidural, Induction, oligohydramnios, One emergency caesarean, PND, VBAC
Episode Sponsor
This episode is brought to you by the Bonds New Damn Dry Undies.
Did you know that one in three women experience light bladder leaks? If this is you, you’re not alone. That is why our friends at Bonds have created their new Damn Dry Undies. These amazing undies are made with comfy, Aussie cotton. You wash them just like normal undies, and they look just like normal undies. They even have odour control. (Pretty damn smart, huh?)
You can try them out for yourself. Get 25% off Bonds new Damn Dry® undies when you shop at bonds.com.au and use the code ABS25.
Offer only available at bonds.com.au until 30th September 2022. Terms and conditions apply.
Categories
Related Products
-
Birth Combs: Harness Your Body’s Natural Pain Relief
$24.95Crafted from smooth, natural wood, our birth combs activate specific pressure points in your hands that trigger your body’s innate pain-relieving responses.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us