Podcasts Sasha
EPISODE 331
Sasha

“Conception was quite intentional for us. We got engaged just as the world shut down for covid and then we decided to flip the tradition and have a baby before we got married. In 2021 we decided to start trying so I went to the GP to get my IUD removed and she also had a good chat with me about my mental and emotional health, as well as my physical well being, so I had blood tests to check iron and Vitamin D and she encouraged me to take supplements.
“Six years ago Jem had testicular cancer and lost one teste so it was in the back of our mind and we wondered if it would have an impact on our fertility. My GP told me to come back in six months if we hadn’t conceived but thankfully I was back in the office within a few months. I got my period a week after the IUD was removed and I was also tracking my basal body temperature with the ovulation tests.
“I was really keen to test early and the day before I tested I got hit by a wave of exhaustion and it was like never I’d experienced before. I was working from home and I had to get off the computer and just lie down. I did a pregnancy test the next day and I got a faint line. That exhaustion was my main symptom in the first trimester; I also had period cramping which did concern me, from about 8 to 12 weeks, but my GP reassured me that it was quite normal and expected as long as it wasn’t accompanied by blood or dizziness.
“Through listening to the podcast I was interested in considering a homebirth model. I spoke to Jem and we really wanted to be a team, and he had fear and concerns about the homebirth model mostly because he didn’t have knowledge around the safety protocols that are built into that model of care. He’s very practical and I wanted to respect his concerns and I was quite open minded and relaxed about pursuing a hospital birth, too.
“I’m a woman of colour and there’s been prejudices in my education, in my experience growing up here, that are both overt and covert. In reading about the sphere of pregnancy and birth, there’s a disparity in the outcomes for women of colour, for Indigenous women and black women and infants. Growing up I’ve had to navigate racism and prejudice and systemic bias. If we could build our own team around us in our own home, that was appealing to me. Jem and I talked at length about our options and his fear would be appeased in a hospital system, whereas my emotional fear and needs could be looked after in the hospital system with continuity of care.
“When you’re growing up, you see yourself represented in particular spaces, you feel welcome, but when you don’t see yourself, you don’t feel welcomed or considered in those spaces. A lot of the content I was consuming in my 20s…there wasn’t much representation of black women. When I was studying, the anatomical examples never showed black people. That experience really informed this new chapter of my life.
“Friends and family had spoken so highly about Frances Perry House and they had a lot of focus on postpartum care as well which was important to me as I have a history of anxiety. I switched obstetricians at about 17 weeks and I immediately felt relaxed and seen; it was a wonderful choice for us. I hired a doula because I wanted that maternal care in the birth space and she really provided us with a very safe space to take stock and talk about our pregnancy, talk about where we were in our relationship and she provided beautiful, gentle energy to be able to do that.
“I was about 30 weeks when the conflict in Ukraine started and emotionally it just felt like a dark cloud sitting in the back of my mind. We have many loved ones who live there and information was scarce which made it a lot harder. It was around that time I linked in with my psychologist who has been amazing with my anxiety journey since my dad passed away three years ago. At around that time we’d just bought a house and moving while pregnant was so challenging. Jem and I really intended to go inwards in the final weeks of pregnancy, to slow down and really focus on ourselves before Silvester arrived.
“From 36 weeks we were having weekly appointments. He was head down and snuggled in but from 36 weeks he wasn’t engaged; he was descended but not quite engaged. The CTG and ultrasounds were looking really great and I felt really good in myself. Two days before my due date we had an appointment with my OB and the energy was really different and she suggested induction within a few days. A few features that informed her perspective was his size – he was measuring as a big baby – and she noticed there was a bit of calcification of the placenta. I’d done some reading and I knew that at that stage of the pregnancy it was quite normal. However, my amniotic fluid was a bit lower and it’s for all those reasons that she suggested induction. Jeremy and I were really quite floored because it didn’t feel like a collaborative team energy, she just said that this is what was supposed to happen.
“Jem and I asked for some time, we didn’t want to book in immediately. I was in tears. Our doula was fantastic and advocated for us to get a second opinion and we did that. We went to a sonographer and he checked the blood flow through the cord, how he was measuring, the amniotic fluid and placenta and we got such relief because the interpretation was that he was doing really well – there was nothing immediate or urgent about it. With that opinion we went back to our obstetrician and asked to pause and I told her I would be happy to have an induction at the end of 41 weeks. I didn’t want to ruffle feathers and I didn’t want her to feel as though I was undermining her. She was a bit frosty at first but then she warmed up.
“Between that appointment and that next week I did everything in my power to help move my baby along. I’d been antenatally expressing since 37 weeks, I was gutter walking, I was eating dates, I was going laps at the swimming pool, we were having lots of uncomfortable sex, I was getting in all the positions to encourage him to engage. To an extent it worked because when I went back in to see my obstetrician I was 3cm so things were going in the right direction. Every night I had cramps but nothing eventuated.
“We went in on Monday and my OB asked what I wanted to do; the tone had shifted and again it felt really collaborative. I was still hoping I would go into spontaneous labour but on the Wednesday morning I went in for an induction and we were so welcomed by the most amazing midwife. It really helped us let go of our hesitation and we felt really safe and informed.
“The induction process started with the rupturing of membranes and then I had to have the syntocinon drip because he hadn’t engaged. It started on a very low dose and gradually increased. It was such a wonderful experience; Jem had dimmed all the lights, I had my diffuser going and our music playing and our supportive midwife was exactly what I’d envisioned.
“It got to a point where there was no break between contractions and it wasn’t what I expected. Thankfully the obstetrician adjusted the drip and I was having one minute contractions with a nice break in between. This went on for another eight hours and I was still 3cm; regardless of all the active positions I’d tried he still wasn’t engaging.
“After 12 hours of labour I had another vaginal examination and my OB noticed that he was presenting in quite a strange position. We had a conversation around that time and she gave me all my options; I felt really emotionally supported and safe. We decided that a caesarean would be best so they got me into a robe and Jem got in his scrubs and I was wheeled into the theatre.
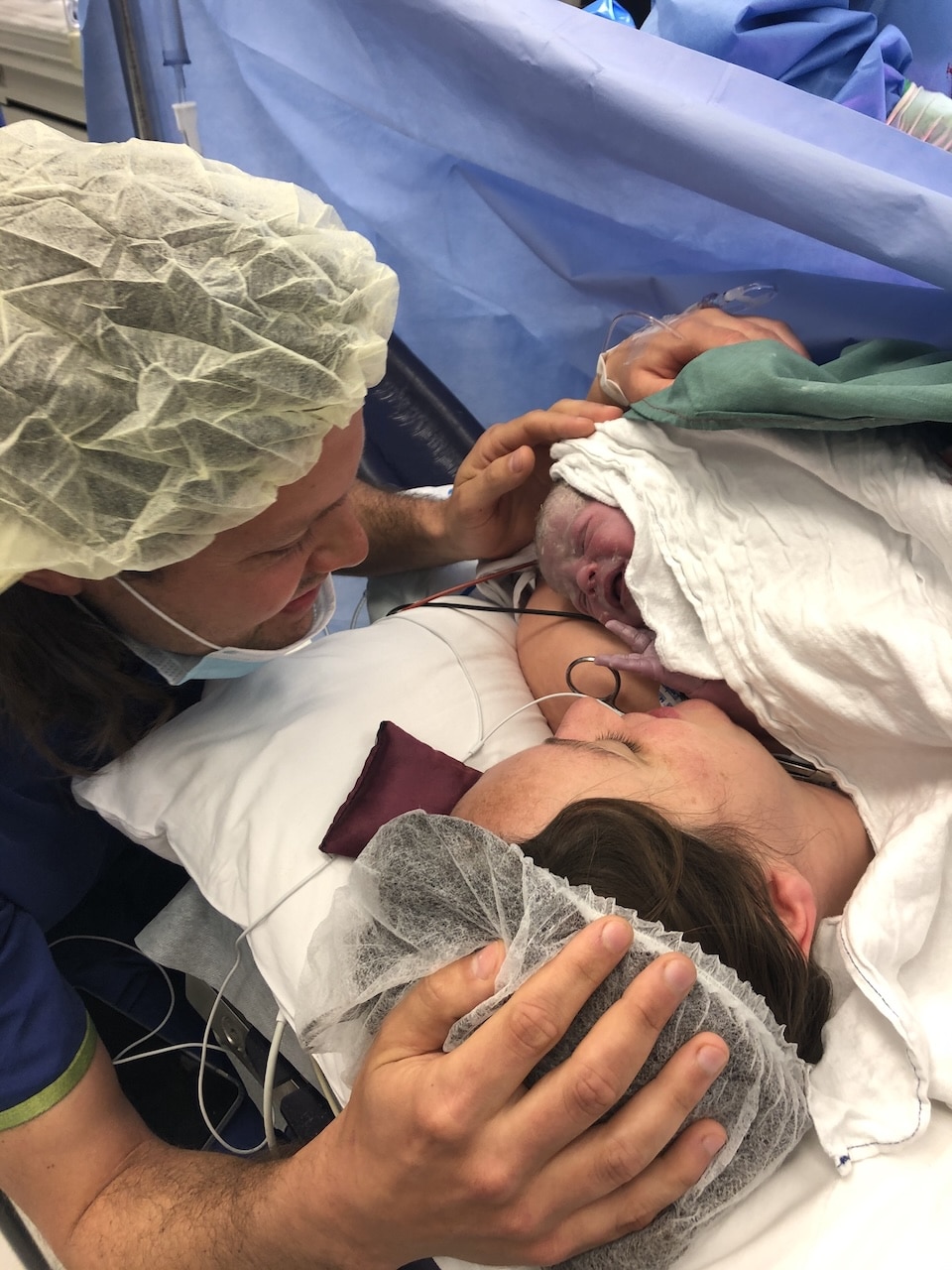
“I asked if we could have delayed cord clamping and skin to skin. The OB was really open to embracing all my preferences and she talked me through everything that was happening. The whole team, from the nurses to paediatricians, introduced themselves and it was such a wonderful atmosphere.
“Silvester was a big baby, he was 4.2kg and his head was off the percentile charts, but when he was born we were all just overjoyed. His head coning was off at a really odd angle which explained why he wasn’t engaged, his big head and the shape of my pelvis meant he wasn’t going to fit. He came out crying and he came to me, we made eye contact straight away and they delayed the cord clamping as much as they could. It was perfect, not what we’d planned, but the best experience of my life.
“We had a physio come in on day two to chat about movement and looking after my scar. The midwives were checking the incision each day and providing guidance around caring for it. I’ve been wearing compression underwear and a belly belt and that’s made me feel more secure so I’m not relying on my lower abdominals. I’ve also been resting a lot and I’m just about to hit six weeks.
“Antenatal expressing set me up for a really good breastfeeding journey because in that process I had the opportunity to understand my own breasts and nipples. The care of the lactation specialists in the hospital was wonderful as well because they guided and encouraged me in those first few days which made me feel really confident.”




Topics Discussed
Continuity of care, Doula, Emergency caesarean, IUD, Private obstetrician, Woman of colour
Episode Sponsor
Today’s episode of the show is brought to you by Expectful.
You might have discovered that pregnancy and postpartum can create stress and anxiety. Even for the most prepared parents. That’s why I’m delighted to tell you about Expectful.
Expectful is the mental health app for before, during, and after pregnancy.
Seriously, this app has so much for your mental health, and it was designed by a team of perinatal experts, holistic wellness practitioners, and mums who have experienced it all. You simply enter your due or birth date and receive weekly custom content throughout pregnancy and postpartum journey.
With Expectful’s free, 7-day trial, it’s a no-brainer to give it a try. And if you use the code either on the app AUSBS25OFF or at expectful.com you’ll get 25% off your annual membership.
Go to expectful.com today to start your free trial.
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us