Podcasts Avril
EPISODE 330
Avril

“I immediately knew I was pregnant; it’s so hard to explain but I intuitively knew that I’d fallen pregnant that night. I did a test 12 days post-ovulation and it was negative so I got in the bath and when I got out I noticed that there was a very, very faint line. The next morning another test was very much positive.
“I had a really great GP who I had a good relationship with and she knew that I had private health insurance so she suggested that a private obstetrician she knew of would be a good match for me. I was very sick, I got to a point where I was throwing up 15 times before lunch. I just thought it was morning sickness and at that point I was working from home so I rested where I could…I didn’t feel it was impacting me that much but then I called the midwife at the obstetrician’s office and she got a restavit script written for me and that really helped, although I was still vomiting a few times a day till 35 weeks.
“At 26 weeks my baby was diagnosed with Intrauterine Growth Restriction (IUGR) and we had scans weekly from 30 weeks. The conversation was just one more week, it was a watch and wait situation. The induction conversation came up, as well as the conversation on whether I’d be able to birth vaginally. I was closely monitoring his movements at home and then we got to 38 weeks and it was a huge relief. My obstetrician was quite happy to do scans every two days and keep going. I had a stretch and sweep but nothing happened and then at 38+3 I woke with the feeling that my baby needed to be born that day. I asked to be induced and I went in that night and had the cervical gel. My waters broke spontaneously the next morning.
“I was walking around the room and I put my TENS machine on but labour came on very fast. My baby, Finlay, was posterior and the contractions were constant. I was on my hands and knees and I was comfortable there because I needed constant monitoring, and Finlay wasn’t happy when I was in that position, so I got on the bed and once I was there I didn’t get off.
“Since having my second baby the difference in pain of a posterior labour compared to an anterior labour is immense. It’s a pain that catches your off-guard and there was no way I could get on top of it. I had morphine and it definitely had an effect but not to the extent that it was a relief. I got to the point that I wanted and needed an epidural and the relief was immediate. It was a very even and quick-acting epidural. It is so weird to go from being in so much pain to having absolute relief. I had something to eat, I rested, and I had a lovely chat with my midwife.
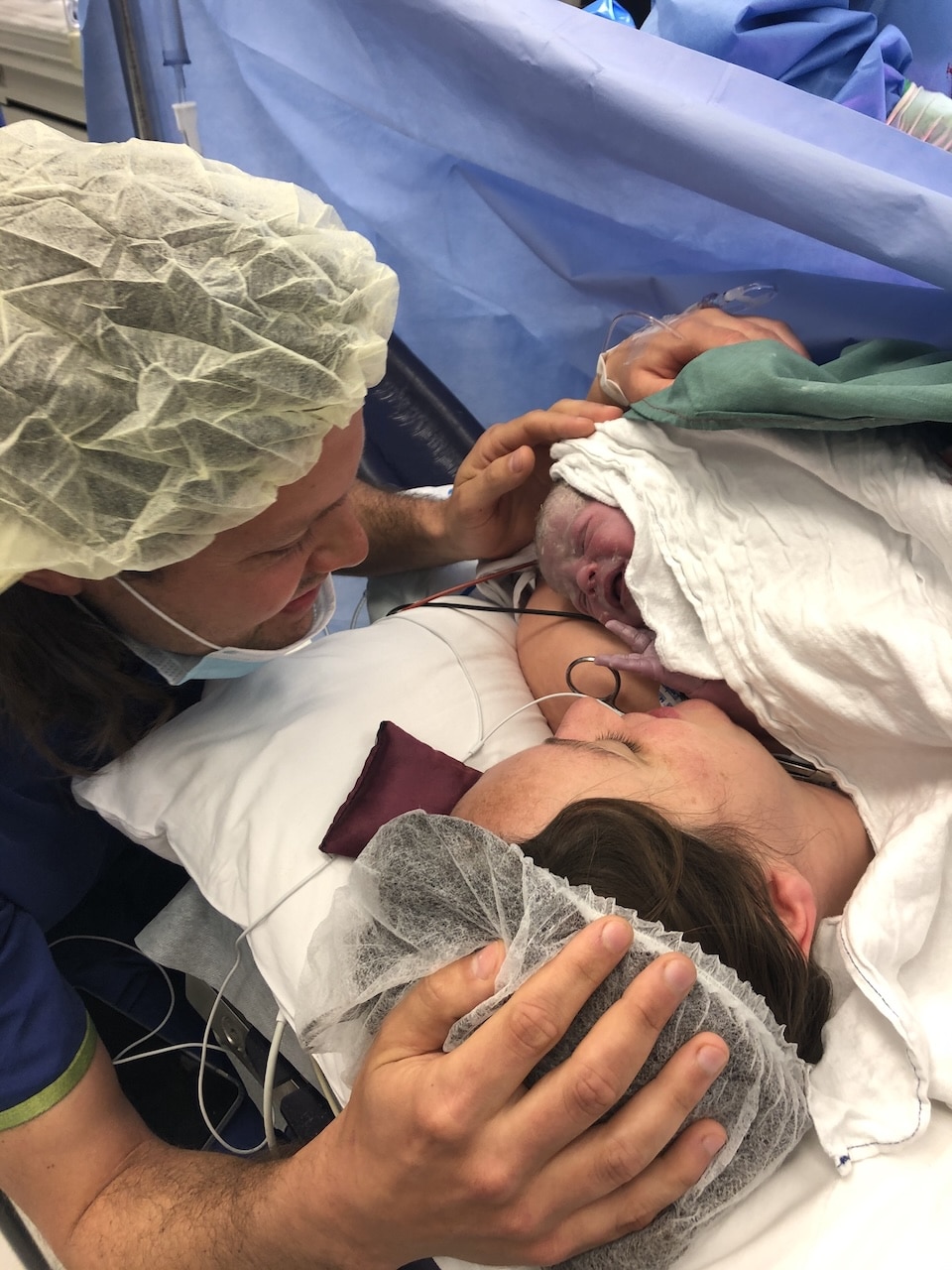
“My contractions weren’t textbook or regular but I dilated quickly, I was only in labour for 10 hours. He was posterior and his head was deflexed. My obstetrician did an ultrasound and she suggested putting the vacuum on his head to reposition it before I started pushing but he immediately moved his head back. It was going to be hard to get him out so my OB suggested an episiotomy and forceps. I didn’t know anything about them but I should have known. In no moment of my birth was I questioning my obstetrician, she was explaining everything very well. I pushed for three contractions with the forceps and there was no movement so they started preparing me for a caesarean. I was determined not to have a caesarean, so I used all the force that I could muster and I pushed and my doctor pulled and he came all the way down in one go. At that point he was crowning and everyone was so elated. He was born soon after and he cried straightaway; he had the grumpiest look on his face. He came straight to my chest and the paediatrician was checking him while he was on me.
I started feeling quite unwell, really faint, and my obstetrician told me I was bleeding but it was “under control, so they gave me IV fluids and I recovered quite quickly. I had a second-degree tear as well as the episiotomy so they stitched me up and then I stayed in that room till I felt well enough to move to my room. I was very wobbly for the first few days and Fin got jaundice so he needed to go under the bili blanket so we ended up staying for six nights.
“I was seeing a women’s health physio in pregnancy because I had a hyperactive pelvic floor which I’ve since learnt is not a great match with forceps. I have a bladder prolapse from my first birth but it’s not overly symptomatic.
“I got my period back six weeks postpartum, despite the fact that I was feeding around the clock. It really shocked me! Falling pregnant was easy the second time and we went back to my obstetrician who advised me to take aspirin regularly to hopefully prevent IUGR. I was diagnosed with gestational diabetes and while I wasn’t expecting it, I was lucky in that I just had to monitor my bloods and not adjust my diet much at all.
“I was induced once my waters had broken and I did ask for the syntocinon dose to be lower than usual, and I only knew to ask that because of your podcast. It was half strength and there were longer intervals between increasing it and labour was all in my front this time which made such a difference. I was monitored with a bluetooth connection so I could stay active; I was walking around, swaying, on the ball – it was great.
“Labour came on gently but I was in active labour within two hours. The monitoring came off and I got in the bath and the midwife checked me with the doppler. I started to get quite agitated and emotional and I went back to my previous birth in my mind. I got out of the bath and I opted for an epidural and again, thanks to the podcast, I asked them to make it weak so while it was effective, I could still feel the contractions and baby’s head bearing down, but with less pain. I was on my side and the contractions got really strong again and I was ready to push.
“I pushed once and I felt him come all the way down and I can’t explain how amazing it was, that level of sensation and awareness that I didn’t have in my first birth. I felt him twist his head and went straight back up and then I did one more push and he was crowning and then I birthed his head and then he was born and I grabbed him under the arms and he came straight to my chest. August latched immediately and stayed on there for about three hours. I didn’t have another bleed this time; my postpartum haemorrhage was a big part of the birth trauma in my first birth.”

Episode Sponsor
This episode is brought to you by the Bonds New Damn Dry Undies.
Did you know that one in three women experience light bladder leaks? If this is you, you’re not alone. That is why our friends at Bonds have created their new Damn Dry Undies.
These amazing undies are made with comfy, Aussie cotton. You wash them just like normal undies, and they look just like normal undies. They even have odour control. (Pretty damn smart, huh?)
You can try them out for yourself. Get 25% off Bonds new Damn Dry® undies when you shop at bonds.com.au and use the code ABS25.
Offer only available at bonds.com.au until 30th September 2022. Terms and conditions apply.
Topics Discussed
Gestational Diabetes (GD), Induction, Prolapse
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us