Podcasts Erin
EPISODE 307
Erin

“My pregnancy was normal up until the day we went for our 20 weeks scan. The sonographer wasn’t forthcoming with information but we noticed that she was taking lots of measurements of Aiden’s kidneys. There were awkward silences and we started to feel that something wasn’t quite right. Towards the end she told us there was something wrong with his kidneys and the amount of amniotic fluid they were producing and we were told the doctors would review the scan and contact us the next day.
“That night was the worst night of my life up to that point. I was madly googling trying to find out more. The next day I got a phone call and it was the most horrific call where the woman from the ultrasound clinic basically told me that there was something significantly wrong with Aiden’s kidneys which affected the amount of amniotic fluid that was produced which significantly affected his lungs and lung development. We had been directly referred to the Royal North Shore maternal foetal medicine unit because we needed to see the specialists there. I remember asking if he would survive and she told me that babies don’t live with this condition and then the phone call ended.
“The next appointment was the next day and we had a 90 minute scan and the whole time I was wondering what they were finding, what we needed to be worried about. We did discover then that we were having a little boy and that the minimal amniotic fluid was affecting the way he breathed which then affected his lung capacity and lung growth. After the scan we met with the maternal foetal medicine specialist and that was confronting because the forefront of the conversation was termination because his prognosis was incredibly poor. When we said we wanted to continue, we were incredibly well looked after and the care we were given was above and beyond, even into my next pregnancy they were still there to support us.
“There was never any 100 percent predictable outcome and Mike and I felt there was a chance that his outcome could be different. We wanted to give our baby the best possible chance of survival which led into the rest of our pregnancy which involved lots of appointments, interventions and additional therapies to try everything to optimise our baby’s outcome. Through the entire pregnancy, birth and even after, I always had hope and there was a chance that we were going to prove everyone wrong. That hope was always there.
“A planned caesarean was the best option for a controlled environment and that was booked for 39 weeks but I went into spontaneous labour at 36 weeks. True to his form Aiden decided when he wanted to be born. The low amniotic fluid caused lots of braxton hicks and an irritable uterus and I’d experienced that for quite a while in my third trimester. My early labour went on for a few days and one day while I was in my local hospital my tightenings turned into full blown contractions so I was taken to Royal North Shore in an emergency ambulance. By the time I got there they had to gather the team together for the emergency caesarean.
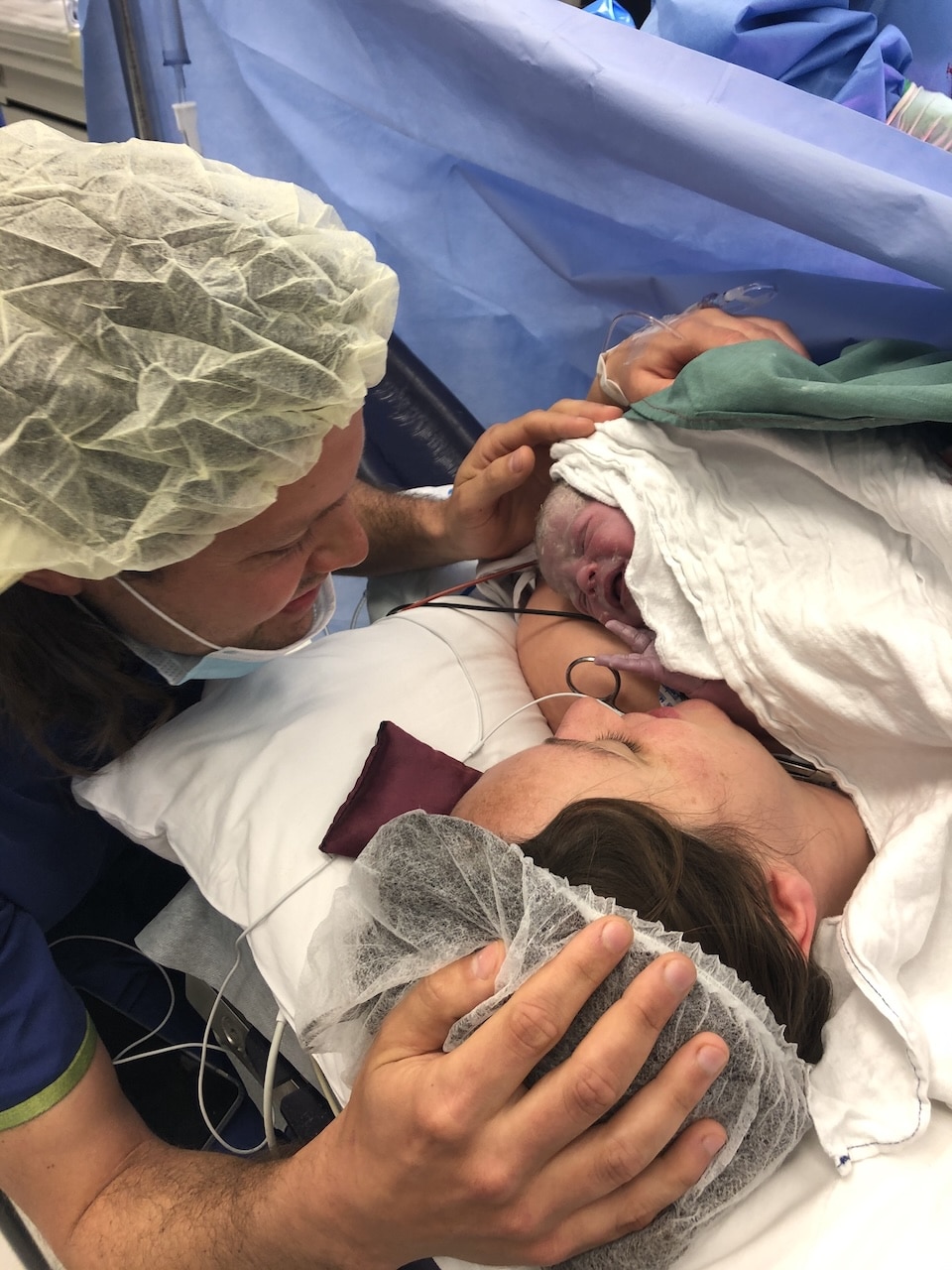
“I just wanted to know what was going to happen with Aiden. I had thought a lot about what he was going to be like when he was born; we knew his lungs were under-developed and we weren’t sure about his urinary system. In yoga I’d created an affirmation that he would come out crying and doing a wee and once he was born he did cry. When I saw him there was no indication at all that internally he had so many things that weren’t normal.
“The neonatal team took him straightaway to intubate him and the neonatal specialist came to see us and to tell us that he was gorgeous and he’d done a wee. I thought he was fine and that he would be ok. It was close to midnight when we got into the NICU, about four hours after the birth. I was wheeled in on the bed and I couldn’t see him so I touched his feet. I thought he was going to be fine.
“The midwives washed me back in my room and I guess looking back I was in a false sense of security. My optimism had grown; I felt so much at ease that I was able to sleep. The next morning Mike went to see the doctors and he came back and that was the turning point. Aiden was with us for 25 hours and all but the last 15 minutes he was in the NICU, hooked up to all the machines you could possibly think of. When I got in to see him they’d done testing and ultrasounds to see what was happening and he was on maximum breathing support. I was standing in front of him and the doctor was explaining everything and she said that was our sign; that was the point that she said we can’t provide any more support. It was just an understanding, that was his sign and we were ready to stop intervention. We had a bit of time to invite family and friends in so they could meet him. They unhooked him from the support and they brought him to us; we went into the room that no parent wants to go to, the quiet room.
“We’d read a book to Aiden throughout pregnancy and we wanted to read that book to us while he was with us. We had that bit of time which again, I’m very grateful for. We had fifteen minutes with him before he passed peacefully in our arms and we told the team that we wanted genetic testing done so after he passed the specialist took a tissue sample. We went back to our room, both Mike and I were able to stay, and for that evening Aiden stayed with us for a few hours and we were visited by family. Mike and I had time with him alone later that night and that was the final time we saw him.
“I asked for a sleeping tablet and medication to suppress my breastmilk. The beautiful team checked up on us and asked if we wanted to see him again but we couldn’t bear saying goodbye again. Walking from the maternity ward to the car was the most horrific experience. I had a box of some of his things that I wanted to keep and that’s what I walked out with – a box, not a baby.
“I wanted to be around people that knew the pain we were going through because no one else could understand. It was such a physical pain, the grief was so physical, my insides were just being torn out. I was in such despair that I called SANDS, their babyloss hotline, and that was the best support I could have ever got at the time. It was the most comforting thing I could have asked for. The woman on the phone was a volunteer that had experienced loss and at the end of the call she told me her experience was so similar to mine and she told me she knew exactly how I felt; I will never forget that. Losing a baby is an experience that changes your life and it was good to be reassured that my feelings were normal.
“So much of our grief was physical; my arms were so empty. It was like my body was telling me that I should have a baby in my arms, my chest was aching. I wanted to try again when we were ready and Mike felt the same. We started trying five months after we lost Aiden and we fell pregnant on the second cycle. In that pregnancy we received the results from the tests and there was no genetic cause for Aiden’s health issues.
“The initial fear was getting through the first 12 weeks and then monitoring how she was growing. We were with the same team so I didn’t have to explain myself which was such a relief. I was able to have scans regularly in the first few months and we knew earlier on that her kidneys were ok. They were confident that I would have a VBAC. I was 40+4 when I woke up with contractions and it was a textbook labour and it was just so different. I went from having a theatre full of people to just having one midwife. She cried as soon as she was born and she went straight on my chest. It was uncharted territory; we were in the same hospital and she was in my arms and we walked out of the hospital with a baby in our arms. It was a surreal juxtaposition.”


Episode Sponsor
The BodyICE Woman Breast Pads, are designed to fit comfortably inside the bra and around nipples to provide cooling or warming relief from soreness associated with breastfeeding, blocked milk ducts and engorgement. The breast pads also conform around the breast pump and when heated, can help ease the flow of milk and blocked milk ducts.
Made from soft medical grade materials and non-toxic gel beads, the packs remain flexible when frozen or heated, are portable and reusable. They also come with washable sleeves that fit around each pack should you choose to use them. BodyICE Woman is available at bodyice.com, as well as many online and retail stores globally. Follow BodyICE Woman on Instagram for lots of great resources and tips: @bodyicewoman
You can enjoy 30% off BodyICE Woman with the code: AUSBIRTH30
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us