Podcasts Kellyanne
EPISODE 259
Kellyanne

Kelly-Anne and her partner Rowan fell pregnant with baby Dulcie in their 11th month of trying. It wasn’t until Kelly-Anne did ovulation testing in preparation for her second pregnancy that she realised she ovulates very early in her cycle, hence her predictions about her fertile window were significantly off. She admits that she spent 11 months concerned about her fertility yet an ovulation test proved that completely false. A little reminder to those of you who are planning to conceive and are unsure of your fertile window (you can buy ovulation tests from the pharmacy, if you’re interested).
“Despite feeling constantly hungover and absolutely exhausted, as in sleeping twelve hours a night and still feeling tired, the most significant symptom I had was being emotionally fragile. I thought that if I wasn’t good at falling pregnant I wouldn’t be good at staying pregnant.”
Kelly-Anne knew the importance of calling her local hospital early to request continuity of care with a known midwife. She wanted her birth to be as natural as possible and admits that she found all the pain relief options to be quite daunting. She attended yoga classes during her second trimester and became really comfortable in her pregnant body; she rocked on her hands and knees to release her lower back, she relaxed while swaying and practising breathing techniques and she strengthened her mind by repeating positive affirmations.
At 32 weeks her baby Dulcie’s head was engaged and Kelly-Anne was diagnosed with significant sciatic pain; she was given a band to wear under my belly and exercised daily to release the pain.
“I was 38+1 and I remember sitting on the end of the bed and I just couldn’t believe how much pressure was in my pelvis. I had a midwife appointment that day and wasn’t sure how I was going to get there. My midwife agreed that Dulcie was right down in my pelvis and she offered to give me a stretch and sweep but I declined; there was already so much pressure and I knew things were going to happen in their own time. The next day I lost my mucus plug and two days later, after I had napped in the afternoon, I had my first contraction at 4pm. I swayed into the evening and then I started timing them but wasn’t overly prompt with the app so Rowan took over. Within minutes he was saying that the app was flashing and telling us to go to hospital. The contractions were coming every three minutes and I’d have two really strong ones and then a not-so-strong one. I called my midwife and the back-up midwife answered and she audibly groaned and told me she’d just sait down after working all day. She told me to stay at home and keep labouring. I was on all fours with my knees really wide and twenty minutes later things had really ramped up so I called back, despite her displeasure and went to hospital. I was the only one in the whole birth suite and the room was so beautiful but I struggled to get back into the rhythm I had at home.
When the midwife arrived she gave Kelly-Anne an internal and stretched her to 8cm. Her water’s broke when she was lying on the bed and the midwife noticed that there was meconium staining which meant she couldn’t birth in the bath and would need to be monitored. Dulcie’s heart rate was going up with each contraction and not going back down but Kelly-Anne was reassured by the midwife that everything was ok.
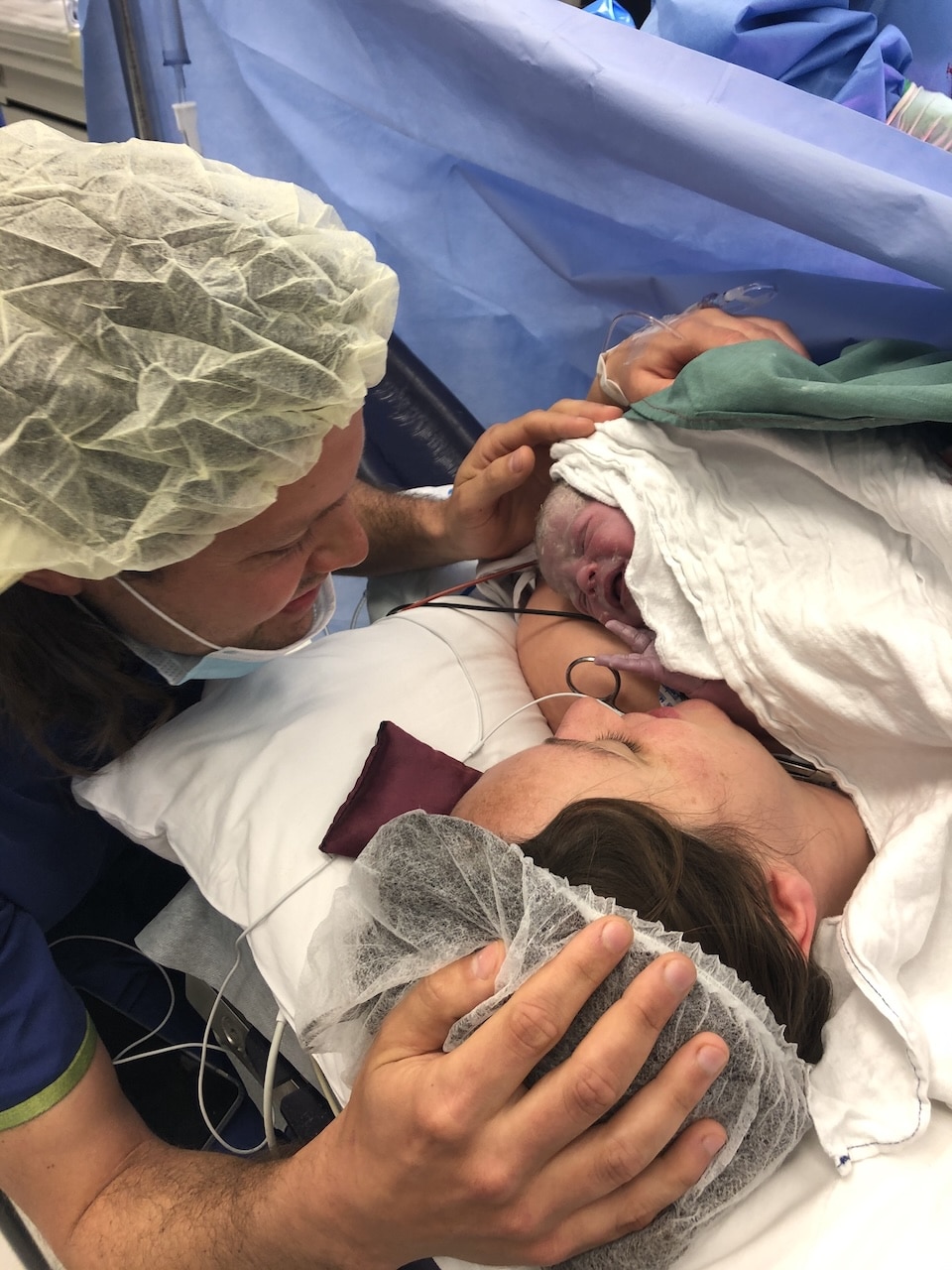
“I got on all fours and leaned into the pillows but Dulcie really didn’t like it so I moved straight onto my back and within minutes the room just flooded with people. They put my legs in stirrups and the obstetrician agreed that it wasn’t ideal but she needed to be delivered promptly. On the next contraction they told me they were doing a little snip and they put the vacuum on her head and the doctor encouraged me to keep the sound in and focus my energy down and on that next contraction I birthed her head. There was a really big break between contractions and the next contraction she was born and she had a really short cord so she was just on my belly. She looked really good, her eyes were open and she was a good colour and when the cord was cut they handed her to the pediatrician and I birthed the placenta and I asked why I couldn’t hear my baby. The midwife brought her over to me and from there she took her back to the pediatricians and that kept going for a while.
“She had a high level of lactic acid in her body and it was decreasing but they needed to monitor her for two hours in special care so Rowan went with her and the midwife told me to take a moment. She said to me: You never even asked, you never even asked for pain relief! Within a few minutes I realised that I couldn’t just lie there while my baby was in special care so I got up and had a shower and went down to see her and we were transferred to the maternity ward at 5am. I stayed that day and one more night and went home and my midwife did my home visits and debriefed with me, which I found really helpful.”
Kelly-Anne regards the first two weeks of Duclie’s life as beautifully blissful. She breastfed Dulcie till 15 months and she was down to one feed in the morning when all of a sudden, she refused to suck.
“One morning she looked at me with a scrunched up face and pushed me away. The milk had obviously changed flavour because I discovered I was pregnant soon after. I was really daunted at the thought of giving birth again but I got through that, comforted by the gratitude that I was giving Dulcie a sibling. I was so sick; I never vomited but I just felt so awful all the time.
“As I entered my third trimester, everything got more challenging, but that’s not abnormal for pregnancy. I felt as though my baby wasn’t sitting properly, I felt really squashed and that my belly wasn’t stretching as fast as my baby was growing. I was just getting more and more lethargic and feeling unwell and I just felt so incredibly uncomfortable. I just couldn’t work out where she was sitting and I had a lump on the upper right side of my belly that was sore.
By 34 weeks I had no appetite, I was shattered and absolutely exhausted. I had a shower one evening and I said to my husband: Do you think I’m jaundice? I looked like I’d had a cheap spray tan which was odd considering I hadn’t spent a lot of time in the sun; the bushfires during summer meant we couldn’t go outside and then covid hit. I thought I’d make a conscious effort the following day to get some sunshine and eat well.
“I was 36 weeks when I went to my midwife appointment with raging reflux and sciatica. I explained that I didn’t feel quite right and the midwife took my fundal measurement which was 32cm, significantly less than it should have been. She took into account my concerns and said she trusted my intuition and she gave me a referral for a growth scan. Later that morning I went to the physio for my sciatica and when I got home I was shattered and just couldn’t comprehend the depth of my exhaustion. I went to bed really early and Rowan came in at 9pm and I started vomiting all of a sudden. I did wonder if I was in early labour.
“I didn’t have much of an appetite but I was drinking a lot yet whenever I went to the toilet my urine was so yellow which was strange considering I was constantly drinking water. I remember looking at my hands in the bathroom and thinking they looked really yellow, too. At 4am I started getting contractions. I waited till 7am to call the midwife and I shared my concerns but I told her I was having contractions every 2-3 minutes but they were really mild. It felt like things weren’t adding up so I said I wanted to come in and just get checked and I reiterated that I was more than happy to come home again.
“At the hospital my midwife, the same one I had seen the day before, got me up on the bed and put the monitor on me; one to measure contractions and one to measure Evelyn’s heart rate. She also gave me a button to press whenever I felt the baby move. She came back twenty minutes later and I hadn’t pressed the button and she was a bit concerned about Evelyn’s heart rate. The next time she came in with an Obstetrician and they both commented on the fact that they weren’t happy with the trace; despite having contractions every few minutes, Evelyn’s heart rate was staying the same; she wasn’t responding to the contractions.
“The OB asked to do a quick internal and he did. He scratched the top of her head and she didn’t react at all so they rushed me straight to theatre for a caesarean. I was there within two minutes. There was a midwife who had the most beautiful face and she was asking about my birth preferences and if I knew the gender and I felt so confident with her and I asked about what would happen after birth. Hospital policy was that mum and baby stay together in recovery which I was really happy about. The epidural went in quickly and the midwife told me that Evelyn was going straight to the pediatrician and there was just silence, everyone was just staring over there at the resuscitation table. I had to ask them to tell me the gender. They asked Rowan to go over and cut the cord and he came back to me and he just laid on the ground.
“The midwife insisted that the pediatricians show me my baby so they stopped the crib beside me but it was higher than my bed and all I could see was a little blue ankle. I knew then that it was so much worse than I first thought. That’s where my memory ends. I can’t remember the end of the surgery or recovery. My next memory is being wheeled into the maternity ward and the midwives were so lovely and gentle; they cleaned me so I could go and see my baby.
“I was wheeled into special care and Evelyn was being treated in a room where my bed couldn’t fit. I was really supported on that first day, I had a social worker come to me to talk through things. I was assigned my own midwife and she looked after me, got me food and told me she would do my observations every hour.
“The doctor explained that Evelyn had meconium aspiration, she’d filled her waters in a state of distress with meconium and had taken a breath, or a few, in the womb and she’d subsequently filled her lungs with meconium so she couldn’t breathe. She was on 100% oxygen and she was very very sick. Despite everything, I had an unwavering sense that she was going to be fine.
“The NETS (Neonatal Emergency Transport Service) flew in to stabilise her and then transfer her to a tertiary hospital with a NICU. I didn’t learn till she was three weeks old that she was without oxygen for 12 minutes after birth and to be honest, I’m glad I didn’t know that then. They transported her at 7 hours old and Rowan went in the helicopter with her. Once she landed I was allowed to be transferred by ambulance and my midwife went with me. Before I was transferred I had spiked a fever so the hospital gave me IV antibiotics and took my bloods. The tertiary hospital was supposed to check on the results. Unfortunately, in the changeover this information wasn’t prioritised but it would have alerted my care providers to just how serious my condition was.
“It wasn’t until the next day that I got to see her, once my spinal block wore off and I had pain relief and they had taken out the catheter. She was 24 hours old. She was the priority baby, she couldn’t breathe and she was just covered in tubes. I held her hand and just stared at her. I was going back and forth between my room and NICU, going back for pain relief and food and to pump and I realised that I really wasn’t feeling well at all.
“Evelyn was on mechanical ventilation for 22 hours and cpap for 25 and by the time Thursday afternoon came around all respiratory support had ceased. She was doing so well, everyone was just raving about her. One of the NICU nurses asked if I wanted to breastfeed her and she removed her feeding tube and she warned me that she probably wouldn’t suck because she was only 36 weeks but she just latched on like a little piranha and everyone cheered. I was so relieved but I was feeling really off and I was in so much pain. I was getting a lot of pressure built up in my belly and I thought it was just because I had been constipated at the end of the pregnancy. Rowan couldn’t stay at the hospital anymore and I felt the weight of him not being there so I really pushed myself to get to Evelyn for feeds throughout the night. I still couldn’t walk or stand up and I just didn’t understand why my pain was so bad.
“Evelyn was doing so well, she didn’t have any monitors and she was in clothes and having formula feeds and they were talking
about discharging her. I was thrilled but I was also terrified, I had no idea how I would get home. I thought maybe I just needed to get some fresh air or see Dulcie or have a lovely meal.
“Rowan had to help me to the shower one morning, I couldn’t walk or stand by myself, and as I removed the pad that was across my wound a gush of blood fell to the floor. The midwife who was looking after me told me I was fine, my blood pressure was fine and I didn’t have a fever and I probably just needed to rest. The doctor checked me and she said the same. Because I was so exhausted and unable to get off the bed, they put a catheter back in so I didn’t need to go to the toilet.
“My family visited and I vaguely remember them coming; I couldn’t lift my head off the bed. The afternoon midwife came in and was shocked at my condition. She reiterated that I really wasn’t ok, she said no one should need a catheter back in because of exhaustion at 5 days postpartum. She took my bloods and within a few hours the results were in; they moved me to a single room, they made me NIL by mouth, they did more tests and ordered an xray and an ultrasound. At 4am a team of doctors came in to tell me that I was in acute liver failure, my kidneys were failing and my blood wasn’t clotting and I was incredibly sick and they couldn’t work out why.
“I had barely slept for two weeks at this stage and I was having observations done every hour. They moved me to birth suites so I could have constant care and I was taken for an ultrasound. At this point my caesarean wound was openly weeping and it was so uncomfortable but I was just so grateful that it was happening to me and not Evelyn. The sonographer discovered that I had a 350ml hematoma in my abdominal area. They called for surgery and I was prepped for surgery and the waiting game began; I was wheeled to surgery and back again because of emergency caesareans. Luckily Evelyn could leave the NICU to come to my room which really bolstered me. I had surgery at midnight and I woke up in recovery and I felt amazing; the pressure and pain in my abdomen was gone and I went straight back to the maternity ward. I was eating and feeling so much better and that day my parents came to visit with Dulcie and Evelyn was discharged to my room and I was a million times better than the day before.
“Rowan had taken Dulcie to his parents house and my parents and sister were in the room with me. Evelyn started crying and I was so thrilled to be able to feed her so she latched on and all of a sudden I was spiralling, my head was dropping, I had no energy and I couldn’t hold her. They buzzed the midwife and she immediately called the doctors. The doctor asked me how I was feeling and I just said that I felt terrible but I couldn’t explain it. She told me to close my eyes and take deep breaths and she encouraged me to share any info I could because anything could help her understand what was going on.
“I said to her: this is going to sound really dramatic and I’m not a dramatic person but I feel like I’m shutting down, it feels like my body is shutting down. She took me straight back to birth suites, reiterated that I wasn’t ok, ordered another ultrasound and they discovered that there was another hematoma. I was in surgery for the third time in eight days and that time it was quite complicated. I woke up feeling awful. I was groggy, nauseous, thirsty, in pain and exhausted. At this point my sister, a nurse, had checked into the hotel next door. She was tag teaming with Rowan to look after me.
“The surgeons came in to tell me that the surgery was complex and they had put on a post-op dressing with a sponge that was attached to a vacuum pack and it essentially sucks ooze out of the wound and into the cartridge. I felt really trapped on the bed; I had a catheter and the cartridge and it took two people to get me into a standing position. The liver specialist came in to say that they were sure my liver issues were pregnancy related and now that I wasn’t pregnant, the liver had an opportunity to rebuild itself.
“The OB came to see me and she confirmed a few things; the extreme thirst, the nausea, the jaundice were all related. She also admitted that I hadn’t been looked after very well. She gave me a likely diagnosis of Acute Fatty Liver of Pregnancy (AFLP) and explained that it was incredibly rare; she had never had a patient with it and neither had her colleagues. She said she really needed to explain just how sick I was because I wasn’t presenting in the way that my blood results were indicating. Everything was deranged, nothing in my bloods was in the normal range. Healthy liver function is between 5-35 and on that day it was 1111; my liver was essentially exploding inside of me. That helped me realise just how sick I was. The mortality rate is ridiculously high. Of the people diagnosed with this, 75% die. The only thing you can do is birth your baby, you just need your baby out so your liver can repair.
“Evelyn was producing a fatty enzyme that was transferring to me through the placenta and clashing with my liver. My liver couldn’t process it and was essentially exploding. So yes, she essentially saved my life by going into distress and going into early labour.”
Kelly-Anne’s wound dressing was meant to last for seven days but three days after surgery the cartridge was full and the hospital couldn’t find a replacement. They turned it off and decided to wait till the next day. However, leaving the dressing on without the cartridge working can lead to sepsis so Kelly rang the REACH (Recognise. Engage. Act. Call. Help is on its way) number and within minutes she was attended to by doctors and midwives.
“They ripped the dressing off and the wound was looking good so they put a dressing over it and told me I could be discharged. When I left the ward, none of them looked me in the eye. Once I was home and lying on the bed, unable to get up and feeling so unsupported, I had a lightbulb moment. I called my group midwifery team and within an hour my midwife was on the end of my bed as I cried. I was black and bruised over my torso and her face just dropped, she couldn’t believe the extent of my bruising or the severity of the wound. She encouraged me to go straight to emergency and the Senior Doctor there was just as mortified. He called the obstetrician who had performed my caesarean and she was beside me withing ten minutes, telling me that the whole team had been thinking of me as they were so worried. That level of care was just so welcomed. She thought the wound was ok, she was happy for me to go home but she made me promise that if anything changed and if I felt unwell, I should call an ambulance immediately.
“When we got home from hospital Evelyn developed colic and her fussy feeding led to a drop in weight gain. The pediatrician explained how important her physical weight was for her development and he had saved her life, so I trusted him. I asked if she could have formula feeds with top up breastfeeds and he was more than happy with that. I’d offer her the breast if she needed comfort, if she was hiccupy, all throughout the day I would offer her the breast and I’d feed her throughout the night, too. Once she was well established on solid food and the weight gain issue was behind us, I wound back the formula until she was solely on food and breastmilk and I’m still feeding her.
“My physical recovery has been slow but I’m getting there. I also credit my mental health recovery to three
distinct things: breastfeeding success, feeling so proud of Evelyn and I. That euphoric feeling of being able to feed her and know that I can do anything. Secondly, I run my family’s small business, a boutique baby shop called Precious Little and I take Evelyn with me. It’s such a supportive environment and I get to talk to mothers all the time; a woman who had a caesarean on the same day as me, someone whose baby was starved of oxygen at birth. That supportive village made such a difference to me. Finally, my sister went into labour with her third baby two days after Evelyn’s first birthday. I got a text to ask me to come to the hospital and I didn’t know what that meant so I went into the birth suite not knowing what I was walking into. She was in the bath in late stage labour and she stood up in the waters broke into the bath and the visual of seeing the clear waters was so important to me because both my girls had meconium in their water. I loved it. I was right next to the midwife watching the baby’s head crown and I was so excited. I could see the baby’s face before she was even born, in comparison to not being able to see Evelyn’s face for 24 hours. I’m so grateful to my sister for giving me that redeeming experience, there was nothing negative there. It was the most amazing moment and I’m so thankful to my sister for giving me that redeeming experience. It was a beautiful form of closure.”



Topics Discussed
Acute fatty liver of pregnancy, Meconium, Spontaneous labour, Two births
Episode Sponsor
BabyDink is the original all-in-one newborn carrier. Known as the ‘no wrap wrap’ BabyDink is a game-changer in those early months of parenthood. Simply worn like a top, there is no origami video tutorial needed. BabyDink is easy to use, safe and supportive for both the wearer and bub. Designed for the first 6 months, BabyDink is perfect for kangaroo care, babywearing and skin-to-skin contact for even the tiniest babies. Enclosing and soothing your baby during their ‘fourth trimester’.
The weight of your baby will be distributed evenly over your upper body so it won’t tug on your shoulders or back, and the specialised organic fabric is pre-shrunk to ensure no sagging or stretching out of shape. The organic fabric is specially knitted for BabyDink in Melbourne Australia, beautifully soft, breathable, and available in a range of shades that will make you look as good as you feel. It is also the first carrier to cater for all sizes 4-24 AU, making it a favourite among both mamas and papas. You can enjoy 15% off your first BabyDink purchase with the code: ABS15 at checkout, head over to BabyDink to see their full range.
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us