Podcasts Jacqueline
EPISODE 253
Jacqueline

Jacqueline’s first pregnancy was a total surprise. “It was the best curveball life could have thrown me.” She was 26 at the time and studying nutrition; a baby definitely wasn’t on the cards. She embraced the pregnancy and joined the Midwifery Group Practice program at the Royal Women’s in Randwick, did a Calmbirth course and actively prepared for her birth despite the fact that she was the first of her friends to have a baby.
“I went public with all three pregnancies and I couldn’t vouch more highly for the service they provide. I got into a MGP with Jet which was really well supported. It was my first pregnancy so I was naive but it was a great experience and they were really open about the fact that every pregnancy, labour and birth is different and you have to be willing to go with that. I went in with an open mind but I was also quite stubborn, I didn’t want pain relief and I ended up having a water birth with him. It was really special.
“I had a show and after going to hospital they sent us home and I went back the next day; there were showers, rolling on the ball, getting in the bath and doing what felt most natural. I birthed him in the bath and Jet’s father caught him, which was really powerful. It was a really special way to bring him into the world.”
Jacqueline admits that she didn’t know, or had perhaps forgotten, that she had to birth the placenta. She experienced full body shakes during delivery and was overwhelmed by the process, shocked by the primality of it. When it came to breastfeeding, she’d done her research but she wasn’t prepared for the emotional and mental toll of the first few weeks postpartum.
“The way that we speak openly about pregnancy, breastfeeding and postpartum, especially emotional wellbeing, is very different now to what it was a decade ago. I was trying to navigate my way through it on my own because I feel like there wasn’t as much support then, there wasn’t social media so you had to really search for guidance…it was a tough time but we made our way through it.”
A decade later, with her new partner, Jacqueline planned her second pregnancy. After trying naturally for a few months without success, Jacqueline did a few rounds of cycle tracking with Monash University which she admits was really helpful and on the second round she fell pregnant.
“It’s a great way to pinpoint your most fertile window. They take baseline bloods which is the first day after your period finishes. They take bloods at different stages through your cycle and an ultrasound to check follicular growth and then in the lead up to your fertile time frame, they’ll do one more round of bloods and then they call you to say: you’ve got 72 fertile hours, go for it! It’s non-invasive and three rounds are completely covered through medicare. It’s also offered to women who just want to understand their cycle. It’s simple and it’s effective and I highly recommend it.”
Jacqueline couldn’t get into the MGP program because of the influx of pregnant women so she chose GP shared-care. Her waters broke at 38 weeks and after presenting to hospital to be checked, the midwives sent her home and told to return a day later to be induced if labour hadn’t started spontaneously.
“We were induced and because the membranes hadn’t fully broken, nothing was changing. There were three different midwives within six hours and the third one was like the matriarch and she felt like she needed to break the waters to get things progressing. She looked at me sternly and said: you don’t need the epidural, your body knows what to do. Let me break the membrane and you’ll have your baby in an hour and a half. And she was right.
“It was a really unique experience and Al caught her which was really special. Birthing Elke’s placenta was easy, I was more aware of what was going to happen, I was in a totally different headspace and it was beautiful but you definitely have different narratives that play into your experience when you’re birthing for a second time.”
Elke was five months old when Jaqueline started trying for another baby. After trying for a few months without success, she weaned her and then fell almost immediately.
“That first trimester exhaustion was so debilitating and I was mothering two kids, trying to be present with Jet and running around after Elke and I was back at work part-time. I made sure I honoured my body; I was strict with boundaries and I just went to bed early and got the sleep I needed.”
Jacqueline’s baby, Amelie, was frank breech from early on and didn’t turn once the third trimester hit. She tried everything – acupuncture, moxa, chiro and then she started working through what breech meant to her.
“Breech was such a new concept for me to wrap my head around and I knew this was going to be really different. It was around 34 weeks when they escalated it from ‘she’ll turn’ to putting me in touch with Dr Andrew Bisits, a breech specialist at the Women’s. There’s lots of stories of baby flipping right up until the due date and we were doing everything we could but we felt really well supported from the moment we were booked into the breech clinic. It was a very different closure to pregnancy than the other two.
“I was pretty nervous, I was anxious. I reached out on social media and used my community to have that conversation and understand other women’s experience with breech. It was really mixed but I believed that knowledge is power. From the minute I meant Dr Bisits he was the most cool, calm and collected doctor I’ve ever come across. He has decades of experience and he was so clear on what every stage would look like for me. Breech babies are only three percent of all pregnancies and it’s definitely a riskier scarier. He gave me the choice of the ECV external cephalic version where they try to manually turn the baby or proceed as normal….he recommended the ECV to start with and unfortunately, Amelie became distressed halfway and my body was shaking with anxiety, there was something that wasn’t quite right and I felt there was a reason she was breech, and she wouldn’t turn. Neither Al nor I were prepared for how emotionally draining the ECV would be.
“Dr Bisits gave me my options; he got the pelvis model out and talked me through what frank breech (bottom first, feet up near chin)would look like, how she would turn a
nd be born – her bottom, then leg, leg, shoulder, shoulder and her neck and head out last. He told me to go home, look at some breech birth videos through Breech Without Borders and he said it was my birth and my decision and if I wanted, I could opt for a caesarean. But he reiterated that I’d had two straightforward vaginal deliveries and I was fit and healthy and therefore, a prime candidate.
“Being given choice was incredibly empowering because I know from speaking to women who have had breech babies, there are a lot of obstetricians who refuse to deliver breech vaginally. I knew I was in a fortunate position to be given that choice. In equal parts I found having to make that choice really hard. I didn’t want to have to make a choice.
“Dr Bisits gave me a sweep and nothing really happened. It was my longest pregnancy yet so he got me to come in that afternoon and he gave me a more industrious sweep, he sensed I’d go into labour that night. Sure enough, my waters broke that night and I went into labour relatively quickly. Dr Bisits had been clear that the minute I had contractions I needed to call him; I had his mobile number and he told me to call him no matter the time. We were at the hospital within ten minutes and there were four people waiting for us immediately, a speciality team and we just felt so looked after. I was still really anxious at that point but they were incredible and the team was brilliant.
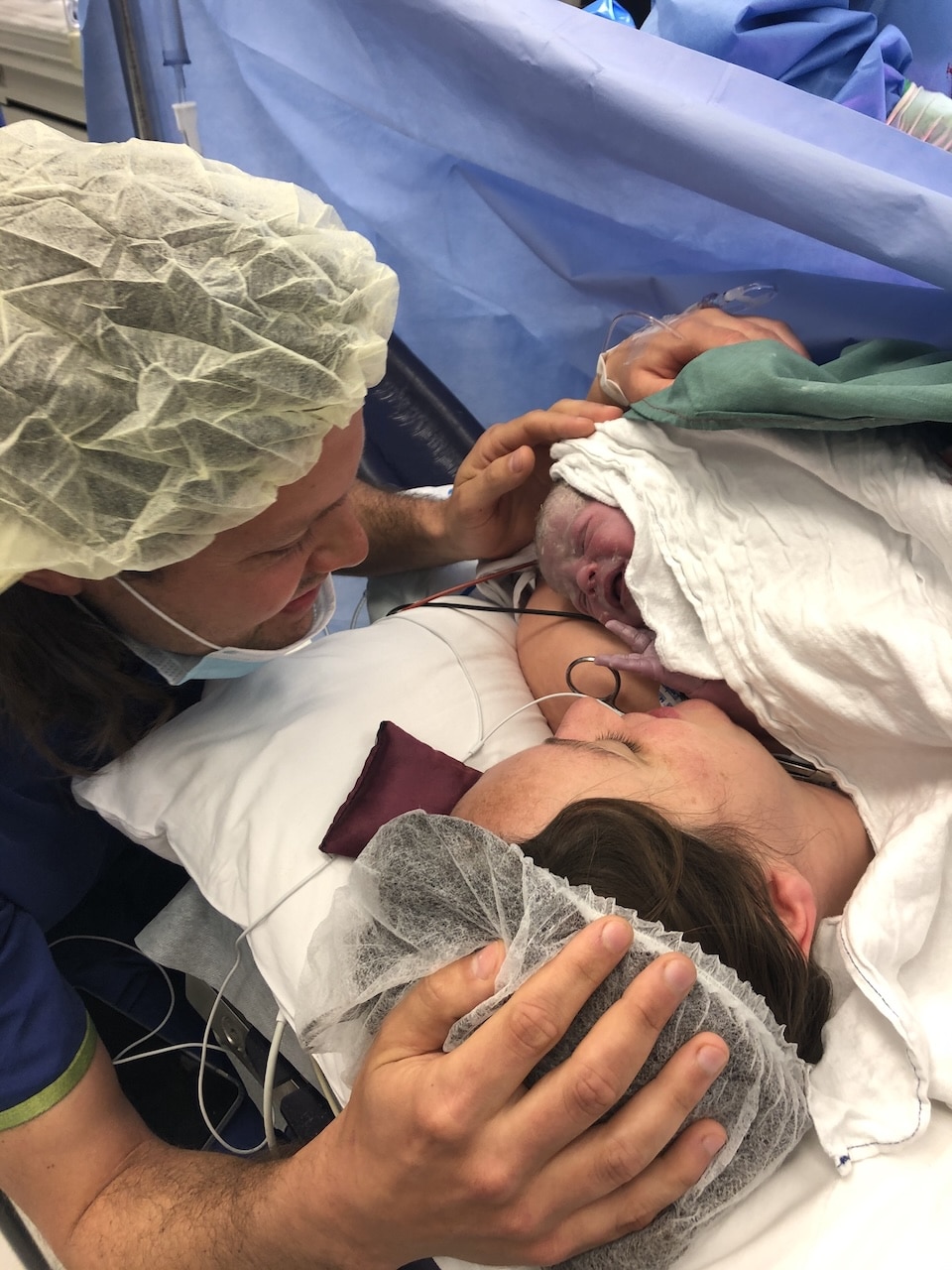
“I made a conscious choice to have an epidural and at 1am Dr Bisits came in, told me I was 10cm and on the next contraction he encouraged me to push. Her cord was around her neck which is why she wouldn’t turn and she was so wide awake as soon as she was born. The anxiety I experienced around the safety of a breech vaginal birth disappeared, I had the team around me to support me and they were all wonderful in the process.”


Topics Discussed
Cycle tracking, Three vaginal births, Vaginal breech, Water Birth
Connect
If you’d like to connect with Jacqueline head over at Brown Paper Nutrition HERE
Episode Sponsor
Today’s episode is brought to you by Modibodi. Voted the #1 Period & Incontinence Underwear Brand, I love my Modibodi undies and I’m excited to share their NEW maternity and postpartum collection which has just launched! I love the flexibility of sticking on my Modibodi undies when I’m not quite sure when my period is coming since my cycles return post-birth. They’re also a fantastic alternative to other menstrual products on the market if you are suffering from a prolapse!
The new range includes a Breastfeeding Bra and Cami with a moulded cup that absorbs milk so you can wear it without any disposable breast pads at all. The best bit is both looks and feels like your favourite everyday bra and give you a great shape, which is a big confidence booster when your body might not be back to its best. The bra and cami both have all your favourite features like easy feeding clips, adaptable sizing and secret support, plus they’re wire-free so you can wear them to bed whenever you can sneak in a nap.
The new range also includes a Maternity Brief with built-in protection for postpartum bleeding – a great idea for your hospital bag – and a Postpartum Control Brief which combines the firm control benefits of shapewear with an absorbent lining for bleeding or a leaky bladder. Ready to ditch the disposable maternity pads and soggy breast pads once and for all? Use the code BIRTH15 to get 15% off your order at Modibodi.com
Categories
Related Products
-
Birth Combs: Harness Your Body’s Natural Pain Relief
$24.95Crafted from smooth, natural wood, our birth combs activate specific pressure points in your hands that trigger your body’s innate pain-relieving responses.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us