Podcasts Em
EPISODE 243
Em

“Henry was conceived while we were on holiday in the UK. All of our friends and family had gone through the public system so we presumed that’s what we would do. We were in Sydney at the start of the pregnancy but we were moving back to Melbourne so by the time we had moved, even though I was so early on in my pregnancy, I missed out on the midwifery led care program at the Royal Women’s Hospital and they suggested I do shared care with my GP.”
Once Em had found a female GP at her local doctor’s surgery, the nation-wide lockdown began and the rest of her appointments were done over zoom until her third trimester. In hindsight, it was this lack of contact and subsequent lack of reassurance that prompted concern and anxiety for her.
“You don’t want to be dramatic and I was very low risk but I think I was quite anxious about the fact that I didn’t get to see anyone and no-one got to see me. I didn’t have appointments at the hospital till I was 36 weeks pregnant so I had this worry at the back of my head that I’d need to go to hospital and I wouldn’t know where to go. I just had no idea what the hospital experience would be like or even where the maternity ward was; it was really anxiety inducing.”
Em and her husband, Jamie, did a Calmbirth class via zoom which helped them feel more prepared for the birth and settled some of Em’s worries. She also found the support from her student midwife to be incredibly beneficial.
“We met Hannah on a few different occasions throughout the pregnancy and we chatted about what we wanted in our birth. I felt like she was going to be a great advocate for us. Unfortunately, because of the lockdown, it started to become clear that Hannah wouldn’t be able to attend so I did get sad about that. She was so supportive though, it was lovely having her share the journey and I feel like so many people don’t realise that you can request a student midwife for your pregnancy; they really are an extra support person and they need to attend a certain number of births before they can qualify.
“I got to 40 weeks, had a stretch and sweep and it did nothing. I could kind of tell that I felt physically well; I really wasn’t uncomfortable at all. I had another stretch and sweep at 41 weeks and they did a scan and noticed that the amniotic fluid was low and told me that I would need to be induced the next day. I was pretty over being pregnant and I was desperate to meet my baby. I asked if there was anything else I could do but they really reinforced that it was important that I was induced. Jamie was allowed to come in for two hours for the induction and then he had to leave and could only come back when I was in active labour. We felt relieved that it was happening and confident in the plan; the gel overnight, waters breaking the next morning and then hopefully a baby by the afternoon.
“We went in on Saturday evening and after a bit of monitoring they put the first round of the gel in and I think she probably did a bit of a stretch and sweep at that time and it was quite forceful, I’m sure something shifted after that. Six hours later they came back and they did an internal and said the cervix was opening up nicely so I wouldn’t need more gel and it was after that when I started having mild period-pain like cramps.
“I found it quite difficult to relax in a shared room at the hospital when I regularly had midwives coming to check me. I regretted not being more assertive in asking when I was going to be taken to the birth suite. By 4pm I got up and started climbing the stairs, hoping it would prompt active labour to start. It got to 8pm and by then I realised that I wanted Jamie there and I was starting to feel fatigued and I couldn’t talk through the contractions. It also didn’t feel like a warm and loving atmosphere and I knew I needed the oxytocin flowing through my body. I called Jamie and told him to come in and he arrived about 9pm. Two hours later the midwife asked Jamie to go home and that’s when he spoke up and requested we get taken to the birthing suite.
“When I got there I was 4cm so I was relieved that things were progressing and from there I laboured throughout the night. I had a tens machine on, I was trying to stay active and it just got a lot more intense and each contraction was very painful and difficult for me to work through. At 3am the midwife broke my waters and that’s when the pain really intensified. At 5am they started the syntocin drip but I literally contracted for twenty minutes straight and was in the most unbearable pain so they turned the drip down.
Things got intense and at 5am they put the drip in but I literally contracted for 20minutes without a break so they turned the syntocinon down. I asked for pain relief and although I’d thought I would never have an epidural – because I wanted to feel it all, especially the pushing – I went ahead with it and all of a sudden I had this relief and the world came back into focus. I could see the people in the room, I could chat to the midwife who had been there for hours and I felt like I was going to be ok.
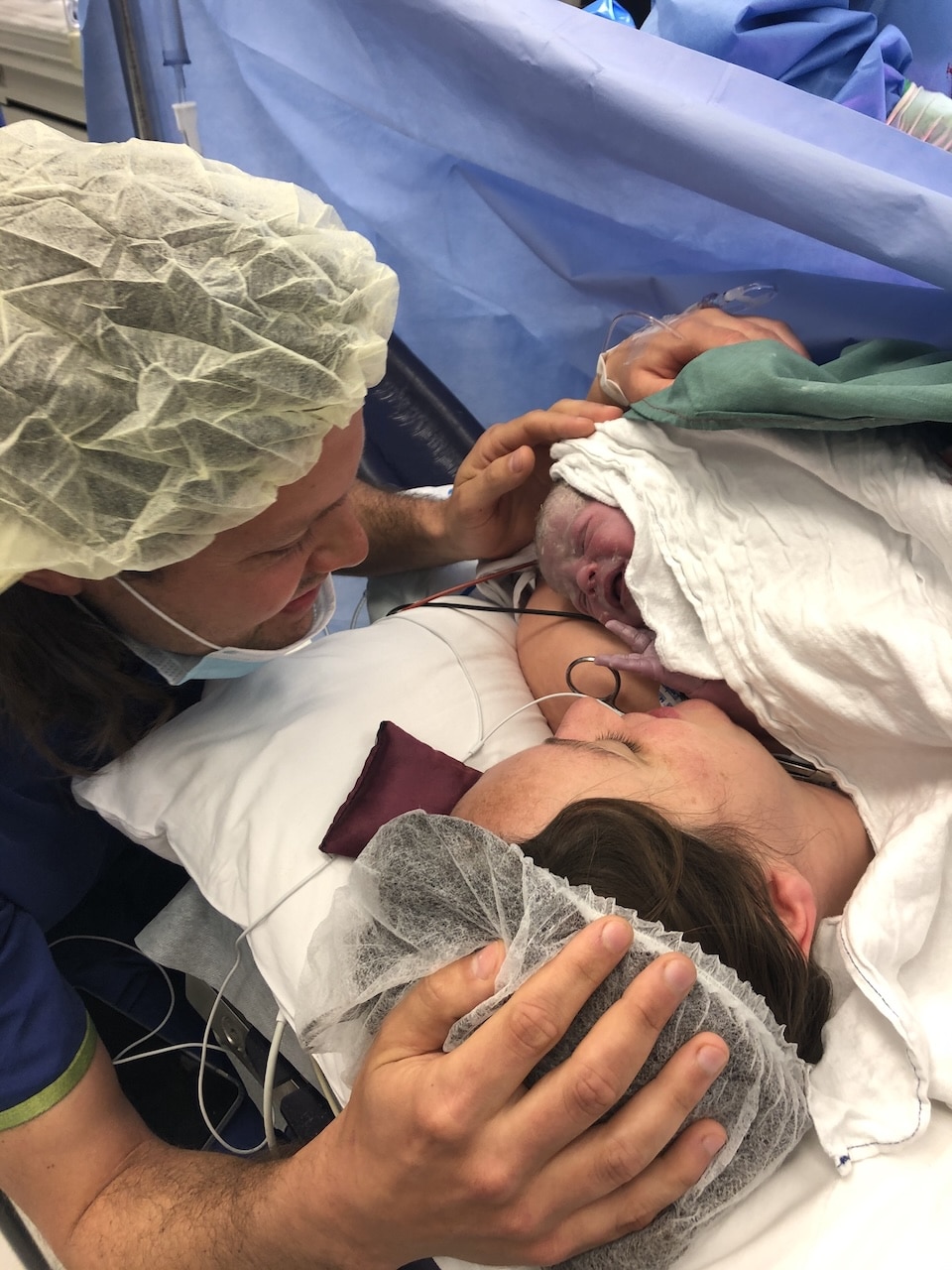
“People talk about the cascade of intervention and I knew it existed but it’s different when you’re in it. After the epidural I pushed for two-and-a-half hours and the doctors were concerned about the baby’s heartrate when I was contracting. They suggested an episiotomy and vacuum delivery. I was relieved but also shocked that my birth had been everything I didn’t expect from a medical perspective. They lifted Henry up on to my chest and I felt a huge wave of relief.
Jamie left a few hours later and I just remember the dread; I was all alone and I had no idea what to do. I got to the end of my labour which felt like such a marathon and it felt like someone lifted up a curtain and said right, you’ve finished that marathon and now it’s time to start the next.
After an anxious first night, Henry was taken to special care for 48 hours but after a slew of tests, was discharged without any diagnosis. Em admits that it was a tough birth made worse for the fact that she was alone for the first few days afterward. But nothing could prepare her for the challenge of the first few months without any village to rally around her.
“When I got home I felt like I had no idea what I was doing and it’s 24/7 so I couldn’t get any break. It built up for me over the next few months and at four months when he hit the sleep regression stage, I realised that my thoughts and feelings that I’d had from the beginning, were probably not normal. I cried a lot, I felt sad and down, I had lots of thoughts of running away and getting away fro
m this life that felt so claustrophobic.
I had an appointment with a GP and she admitted that it sounded like I had had a rough time. I had a breakdown in her office and spoke a lot about my feelings and how I had failed the birth. I thought that motherhood would be mostly joyful with some challenges, but for me it was mostly challenging with small glimpses of joy every now and then. She diagnosed me with PND and PTSD.
“That conversation was life changing because she referred me to Mitcham Private Perinatal Mental Health Unit, often referred to as a mother baby unit. It’s set up purely to look after mums and babies who are struggling. It was really difficult to accept that I was someone who would need that; I had never struggled with my mental health before. But I was in such a dark place that it felt like a reprieve.
“That said, I was picturing a place where people were really unwell and that they’d be walking around in straight jackets…but that’s just the stigma of mental health. When I got there I met five other women who were high functioning, professional women who had children and found things to be more difficult than they ever imagined.
“Going there was completely life changing; I had 24/7 support from psychologists, psychiatrists, amazing nurses who are baby whisperers (and mother whisperers) and these five other women who were going through the same things as me. We did group counselling sessions and I realised that so many mothers are facing these challenges and finding it hard but not openly discussing how hard they’re finding it.
“I expected to be there for five days and that I’d come home and everything would be fixed. Most people stay there for four or five weeks and throughout that time you are absolutely cared for and nourished. You can leave at any point but they encourage you to stay till you really do feel comfortable going home.
Three days after her GP referred her, she walked through the door to Mitcham. Thankfully, she discovered that her private health fund had a mental health waiver, which meant she could increase her health care premium and attend the private health unit at no cost. Em is intent on sharing this information with new mums because it saved her and, unfortunately, it’s not a resource that’s widely known, even in medical circles.
“Coming to terms with my PND and PTSD diagnosis was difficult and it was challenging when we both realised I would be hospitalised in a psychiatric ward but it wasn’t long before we realised how incredibly beneficial it was for me.




Topics Discussed
Epidural, Induction, One baby, Peri-natal mental health unit, PND, Postnatal depression, PTSD, Shared care, Student midwife, Vacuum delivery
Episode Sponsor
Categories
Related Products
-
The Birth Class
108 reviews$249.00The empowering online childbirth education program that will help you confidently prepare for birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us