Podcasts Annabel Bower
EPISODE 198
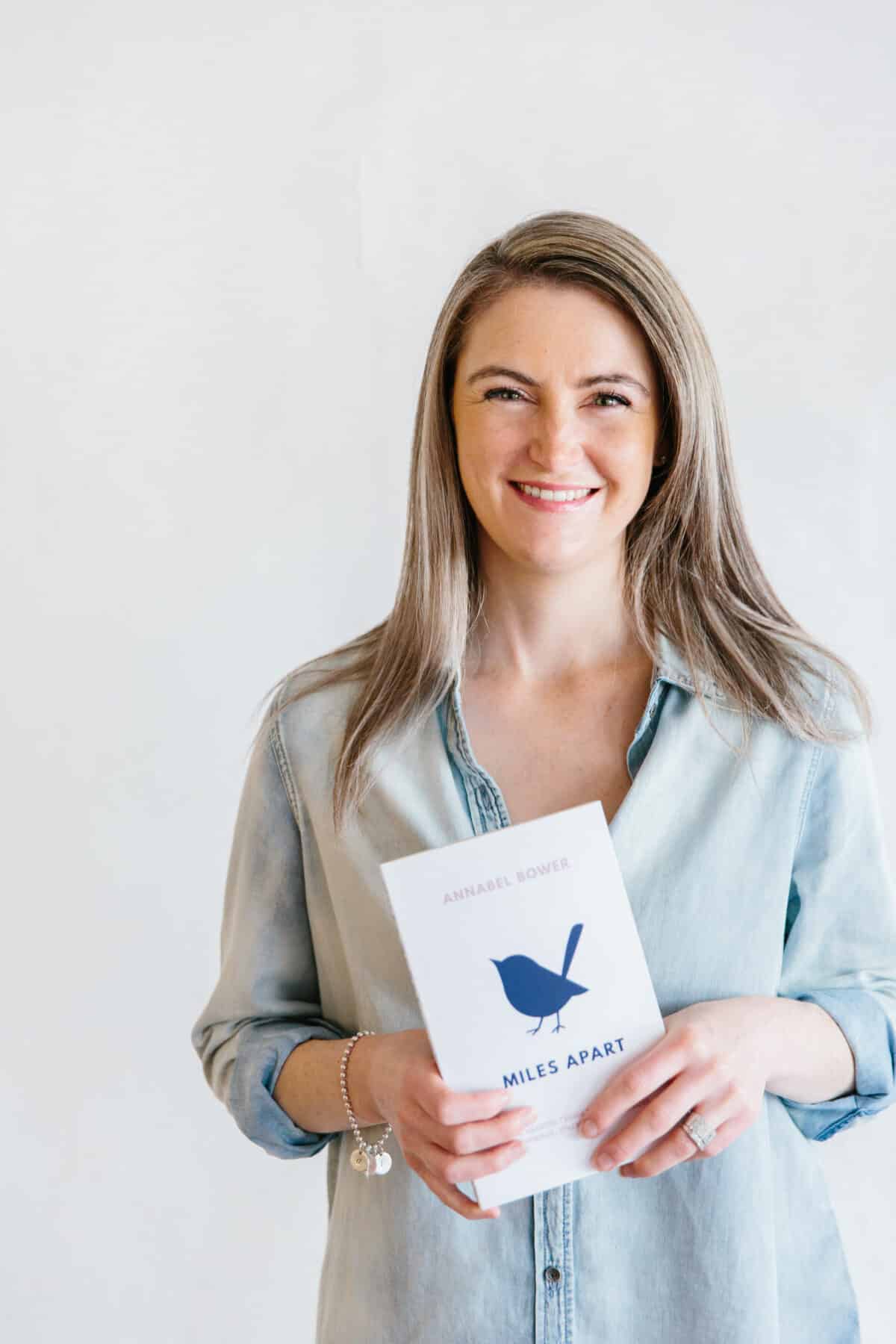
Annabel Bower

You can follow Annabel’s story at @miles_apart. If you would like to donate a book to a hospital or a support service so it reaches the bereaved women who need it most, visit milesapart.online/foundation
Annabel’s first pregnancy, with baby Alfie, was easy, straightforward and blissful. She had no symptoms, didn’t suffer nausea or exhaustion and yet because she was the first of her friends to fall pregnant, she focussed all of her energy on researching cots and prams without actively preparing for birth or breastfeeding. Her birth ended with an epidural, episiotomy and forceps delivery and left her feeling a little shocked by the intensity of the experience. However, Alfie latched easily, she recovered after four months and she discovered she was pregnant with her second son, Ted, around Alfie’s first birthday.
“Ted was conceived without much fanfare which was a welcome surprise. I again had a very straightforward pregnancy till about 36weeks when I noticed a change in his movement, he’d gone from being quite a busy baby to being quiet and I had a gut feeling that something was wrong.”
Annabel went for a scan at 38weeks and it was discovered that her placenta was failing so she was induced. He was born at 2.5kg and couldn’t regulate his temperature or blood sugar and was quite jaundice.
“I wanted to avoid the episiotomy and the forceps and while I had the epidural at the beginning I let it wear off for the second stage. I felt really in control of the contractions and the pushing. The recovery was completely different, I was up walking and doing everything within a few hours and it allowed me to just focus on Ted instead of being consumed by my recovery.
“The boys are from my first marriage and my next three babies are with my husband, Josh. We feel pregnant with Bonnie easily and yet at 11 weeks I became severely ill with pyelonephritis. I was in Sydney at the time and was immediately admitted to hospital as I was almost going into organ failure with blood poisoning. When I returned to my doctor in Adelaide he told me that he didn’t expect to see me with a baby as most women who have this illness miscarry.”
Annabel was fearful and hyper-aware for the rest of the pregnancy, especially as Ted was growth restricted towards the end of the pregnancy. At 26weeks she discovered that Bonnie was slowing in growth and by 30weeks the scans were so bad that she was given steroids and advised to prepare for delivery. “They gave me four days to see if she picked up and thankfully she did and I held on till 35weeks. You’re constantly monitoring the movement and you know that the placenta isn’t working properly and there’s nothing you can do about it. It’s like free-falling, regardless of weekly scans for growth and the doppler for the placenta, you just think well what if they miss something, or what if the placenta fails the day after the scan. It’s not about nutrition, it’s a physiological issue with the placenta delivering oxygen and nutrients which you just can’t control.”
At 35weeks the cord was buffering – what’s coming along the cord is sent back to the placenta instead of being delivered to the baby – and Annabel prepared to deliver. She was induced again but this time via IV and it was a very gentle approach and therefore, a long labour because they couldn’t risk Bonnie going into distress if labour came on quick and fast. Annabel was advised to have an epidural at the start of labour in case she needed to be raced to theatre for a cesarean, to which she agreed.
“Because of her inhibited growth she was treated as a 32weeker even though she was born at 35weeks. She was breathing fine but she couldn’t suck so she fed through a tube for two weeks and then we taught her to breastfeed.
She was in NICU for a month and it was a crazy routine. I’d set an alarm for midnight and 3am to express and to keep my supply up, I’d spend most of my day at the hospital then do the school run, head home and then head back into the hospital for a 7pm and 10pm feed. The nurses and midwives in NICU are superhuman; they carry you through, they keep you buoyed because it’s very easy to get down in that artificial, strange environment.”
Annabel was overjoyed when she fell pregnant with Miles after recovering from the removal of an ovarian cyst. “I was older and a lot wiser, I didn’t announce the pregnancy far and wide because people really tend to comment on having four kids and how busy it would be.”
Despite her happiness, Annabel admits that she couldn’t relax into the pregnancy. She wasn’t sure if it was her age (she was 38) or trauma but she had a gut feeling that something wasn’t right from the beginning and she felt nervous. She had a bleed at 9 weeks but aside from that, everything was going well till her 20 week scan when the sonographer discovered that Miles had a significant issue with his brain.
“From that moment on I knew that this baby wouldn’t be coming home with us. We were referred on to another scan, an amniocentesis and MRI. The first scan was the Tuesday, the next scan and amnio was on the Thursday and the MRI was the following Monday. By this point we had a new OB and he delivered all of the details over the phone. He wasn’t willing to terminate for medical reasons, he’d made that decision early in his career, so we were left in limbo land and I just wondered why we were still dealing with him.
“Miles was diagnosed with severe hydrocephalus, where the brain is filling with spinal fluid, and it’s the worst outcome because the brain hasn’t started developing yet. It made a very difficult time even harder because I felt judged and unsupported by that doctor.
“I was devastated by having to make that choice, it never occurred to me that I’d never be having the baby that I desperately wanted, and if you have a doctor that won’t even meet with you to talk about it you feel immense shame because how can I make a decision if I don’t have all the information.”
Annabel went to her GP who immediately sent a referral to the Maternal Foetal Medicine unit at Adelaide’s major public hospital. Within 20 minutes of the referral being sent she was on the phone to a specialist who talked her through all the possibilities of the diagnosis.
“She told us to come to the hospital and she took us t
o meet genetic counsellors, neonatal neurologists and we went from a situation with zero empathy to an overwhelming team of people supporting us.
“Miles had a brain hemorrhage in utero. Hydrocephalus is usually related to chromosomal abnormalities but he was a very healthy baby who had a hemorrhage in utero and a blood clot had lodged in his brain. It was pretty obvious how serious it was and so we had to choose to deliver him because we knew he wouldn’t survive after birth or if he did, he would have no quality of life, in that he wouldn’t be able to breathe on his own.
“I think I’ve judged myself harder than any person who knows our story, I have never been judged. But in my mind it was such a harrowing decision, I still think of all the what ifs but I know I can’t dwell on them.”
Annabel had to have two doses of medication that would essentially stop the placenta from working and then induce labour. Her labour went for eight hours and she admits that it was as painful and as intense as her other labours.
“The final pushing was a lot easier but the baby doesn’t work with you when it’s already passed. It’s a myth I try to debunk, that it’s not easier to birth a pre-term stillborn baby. It’s an experience that you can’t describe to anyone. You almost want to stop time because you don’t want it to happen, it goes against all instinct to push. It goes against every fibre of your being to bring the pregnancy to an end because you don’t want it to be over.
“The midwives assigned to us were all trained in bereavement and I think it’s an incredibly harrowing experience for them too. I knew how important it was to spend time with Miles and have photographs with him, because once we walked out of the hospital it was all over. It’s a small window of opportunity and you can never get it back.”
She was offered support and counselling from Bears of Hope, SANS (stillbirth and neonatal support services) and Red Nose but she admits that it takes a lot for someone to reach out for help if they’re deep in grief. She was shocked by the grief and the many aspects of it that were debilitating on every level.
“Everything went dark, the fatigue, the exhaustion, the heartache was so intense that it was hard to put one foot in front of another for a long time and no one talks about that. I basically just cried, I just cried endlessly. It was like watching your own life from above, I was doing everything with the kids, but I was completely detached. You feel a lot of pressure to be fine or to be over it, and you don’t want to be that miserable, down friend. I saw a psychologist from the get-go because I wanted someone to be watching out for me because I knew it could be my undoing. I started writing two weeks after I lost him, so I could remember all the details and really bring to light the range of grief.”
Annabel felt that what was most needed for grieving mothers and their families was an immediate source of support that wasn’t medical or clinical but was written by a mother who had lost a baby. A book that could be read by their partner, their mother or their best friend.
“There is so much that needs to be said about this topic and there is so much support that needs to be given and it’s not just for the people who have lost babies, it’s for those around them who want to understand what it’s like and how they can best help. Miles Apart is a gentle guide for women after loss and I discuss all the aspects of grief that are just so debilitating. I wrote what I was thinking and feeling and I think that’s why it resonates with women, because I’m so honest and I’m not writing from a medical or psychological perspective.”
Annabel’s desire to have another baby was almost instant and deeply primal. “it defied logic because those 9 months were the most terrifying of my life. That said, the desire to hold my baby in my arms was always going to be much stronger than the fear.”
She fell pregnant with Tom on Miles’ due date.
“Describing pregnancy after loss is a whole other book and I think I will write it. It’s pure fear that something will go wrong and because we didn’t have any answers and we didn’t know what went wrong, it was very scary. We had a new OB who was beautiful, gentle and kind, he was very reassuring and gave us lots of scans and made us know that his door was always open.
“We had a 16, 18 and 20 week morphology scan and I still hadn’t told anyone, I couldn’t deal with other people’s excitement and I thought people would think it was all good and I could move on, that my sad story was now behind me. Tom was my best grower and my biggest baby, he was induced as the cord did start buffering at 36weeks and my doctor said there’s no point mucking around with me. I went in every day for a CTG and was induced at 38 weeks.
“I blocked out a lot of the labour just to get through it, I knew I would have an epidural and have it up to the max. It was a really calm, nice labour. I’d been ill that week with food poisoning and put on the drip, by the time I had him I was so tired and exhausted that I asked the midwife to take him to the nursery for three hours so I could sleep and when they brought him back that’s when the joy hit.”
Despite advances in technology and a growing (albeit slowly) awareness of pregnancy loss and stillbirth, the rates are still alarming. Miscarriage and stillbirth rates are not declining at all and since the pandemic hit, women aren’t presenting to hospital as often and therefore changes in baby’s movement or the mother’s blood pressure are not being picked up. One London hospital has noted a fourfold increase in stillbirths since the start of the pandemic.
As Annabel says: “It’s an ongoing issue and together I feel that we need to chip away at it. With time I hope it will be easier to talk about and it won’t be met with silence or awkwardness.”


Topics Discussed
Grief after loss, Miscarriage, NICU, Placental insufficiency, Stillbirth
Connect
You can follow Annabel’s story at @miles_apart. If you would like to donate a book to a hospital or a support service so it reaches the bereaved women who need it most, visit milesapart.online/foundation. You can pick up a copy of Miles Apart or Donate a copy to a hospital. To find out more: www.milesapart
Episode Sponsor
This week’s episode is also proudly brought to you by WaterWipes Baby Wipes. When it comes to your baby’s sensitive skin, what you don’t use on their skin is just as important as what you do use. WaterWipes gives you peace of mind knowing that you’re using the best product available for baby’s skin.
Years ago, when founder Edward McCloskey’s newborn daughter suffered from nappy rash and severely sensitive skin, he set out to create what have now become the world’s purest baby wipes. Made with just two ingredients – 99.9% purified water and a drop of fruit extract – WaterWipes have recently been independently tested and proven to be purer than using simply cotton wool and water. In fact, these wipes are so gentle that they’re suitable to use on the skin of premature and newborn babies– and they’re used in NICUs and hospitals across the world. Recommended by midwives, WaterWipes are available online and from your local supermarket and selected pharmacies.
Head to shop.waterwipes.com.au and use the code BIRTH30 to receive 30% off WaterWipes.
Categories
Related Products
-
Birth Combs: Harness Your Body’s Natural Pain Relief
$24.95Crafted from smooth, natural wood, our birth combs activate specific pressure points in your hands that trigger your body’s innate pain-relieving responses.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us






