Podcasts Flick
EPISODE 174
Flick

When Flick hadn’t had a period six months after coming off the pill, her GP sent her for further testing and she was diagnosed with PCOS. She was completely surprised by the diagnosis as she had always suffered from heavy periods. “I had close to 35 cysts on each ovary so I did acupuncture for 6 months but still no period. I decided to see a second OB-GYN who prescribed clomid and discovered that my prolactin levels were high so I went on medication for that and then I got my period like clockwork.”
Regardless of the fact that her period had returned to a regular cycle, she still wasn’t conceiving so on the recommendation of a friend she went to a fertility specialist who drilled holes in her ovaries, a procedure that lets out excess fluid, regulates the hormones and promotes regular ovulation. She fell pregnant the following month but started bleeding at 11weeks. A scan revealed she’d had a missed miscarriage and a blighted ovum (a pregnancy where a sac and placenta grow, but a baby does not) which can be caused my poor egg and/or sperm quality. It was a devastating loss for Flick and she admits that it really shook her faith in her body and it’s ability to fall pregnant.
A few months later she fell pregnant with baby Arnie but experienced on and off bleeding for the first 16weeks which only heightened her pre-existing anxiety. By the 20 weeks scan everything was looking normal, Arnie was growing well and Flick felt confident enough to start enjoying the pregnancy. She chose the midwifery model of care at Monash Medical Centre and was admitted at 31weeks when strong Braxton Hicks became regular and persistent. She was given steroids as a precaution but despite continual braxton hicks she stayed pregnant till 39 weeks. Her waters broke and she presented to hospital with no signs of imminent labour. An induction was scheduled for three days later and she returned home where light tightenings were persistent but petered out in the middle of the night.
When labour started and continued to build in intensity, Flick glided through the contractions and when she did get to the birthing suite, she was delighted to learn that she was already 6cm dilated. However, the OB insisted that induction commence considering it had been over 48 hours since her waters had broken. It was this moment that changed the course of Flick’s labour; as soon as the syntocin was administered she went from being able to talk through her contractions to being completely overcome with pain. “I didn’t know that I had the right to refuse it or to say that I’d like to wait so of course I just went with it,” she says.
Arnie was in a posterior position so her back pain was intense. Sterile water injections – which ended up being the most horrendous pain Flick had ever experienced – failed to work and while she got to 9sm relatively quickly, she got stuck there. The OB tried to manually turn Arnie a few times to get him in a better position for birth but his heart rate started to drop. They administered an epidural to preempt one last manual turn and while Flick believes they gave her every chance to have a natural delivery, Arnie’s decreasing heart rate meant that an emergency cesarean was necessary.
Arnie didn’t breathe independently for 15minutes after he was born which resulted in him going straight to NICU. It was an utterly heartbreaking experience for Flick who had to wait six hours to see him. Thankfully, he was back on the ward with her within 24hours. “When I was pregnant I did a breastfeeding course with the Australian Breastfeeding Association and together with lovely midwives at the hospital I managed to establish a really healthy breastfeeding routine. If you do miss out on skin-to-skin and contact with your baby in that first hour after birth you can definitely overcome it and breastfeed successfully.”
On advice from her fertility doctor who believed that she would have a better chance of conceiving if she tried within a year of giving birth, Flick weaned Arnie at 7 months. It was a decision she regrets as that was late 2016 and she didn’t fall pregnant again till late 2018. During this time she found comfort in infertility and IVF support groups on facebook and spent a lot of time thinking about and researching what she wanted her next birth to be like.
“I had done a few cycles of ovulation induction with injectables, which is low dose IVF medication where they track and see how many follicles you’re producing. They then give you a triggering injuection and then you have sex three nights in a row. I got pregnant after that but the HCG levels were low from the start, despite the levels increasing with time, we ended up on progesterone pessaries to keep the pregnancy going but I miscarried which was traumatic because it was so drawn out. I lost that baby at 8-9 weeks but I’d been getting blood tests done every few days and to be honest it was very stressful.
“I was crying all the time and whenever a friend would announce a pregnancy I just felt awful and then I felt bad for feeling that way…There are a few bulk billing IVF clinics in Melbourne now and it’s only $1500 a cycle. Granted it’s very one size fits all procedure but in our first cycle we got seven eggs and six embryos. We were feeling really positive and we got to day 5 where they transfer the embryo…we were on our way to the clinic when they called to say that none of them had made it. It was horrible, absolutely devastating.”
Flick and her husband, Dave, found a female fertility specialist through one of the facebook support groups and extended their mortgage on their apartment to do IVF through her. “Dave’s sperm was tested and came back as having 0% morphology which basically means that none of the sperm were the right shape. Our doctor said it was an issue that could be rectified with diet. However, before we started a new diet we jumped straight into another cycle and while we got an embryo, it didn’t stick.”
They started 2019 with the intention of doing all they could to fall pregnant. Flick saw a naturopath and started the keto diet which is known to be good for egg quality, Dave started eating meat (he’s vegan) and they both gave up alcohol and caffeine and started exercising regularly.
By the next cycle Dave’s sperm quality was excellent and they got 7 eggs, 5 of which were fertilised (they used both imsi and ivf techniques). “We got to the day of transfer and it came back positive but the HCG numbers were low. However, they were doubling which was positive. But at 8 weeks the scan showed another blighted ovum and I naturally miscarried a few days later.”
“The day we went back for our follow up appointment I knew I was ovulating so they transferred the last embryo. I went to my friend’s house who had just had a baby so I held the baby and we chatted, and that embryo just felt right. We’d nicknamed the frozen embryo, Elsa and then the test was positive, the HCG numbers were great so we knew we were on to a winner from the start. We were discharged from the fertility clinic and we booked in with Monash.”
Flick felt like she wanted more support for her birth and postpartum period this time around so she decided to hire a private midwife who would care for her during her third trimester, assist her at birth and look after her at home for six weeks postpartum. However, two weeks before she gave birth, the state went into lockdown and all her plans for a private midwife literally flew out the window.
“The hospital said I could only have one support person and of course that was going to be Dave. My midwife made the decision not to come to hospital but if we did practise social isolation and pull Arnie out of preschool, she could support us during early labour at home and then during postpartum.”
Flick had a stretch and sweep with the OB at 39weeks and a few days later her waters broke in bed. Her contractions became regular and productive very quickly and on the way to the hospital she was amazed at their strength. There was a Covid screening station at the door to the hospital (they took her temperature and asked her the standard questions about whether she had recently travelled and if she was showing any symptoms) and once she was cleared she walked up to the maternity ward with Dave.
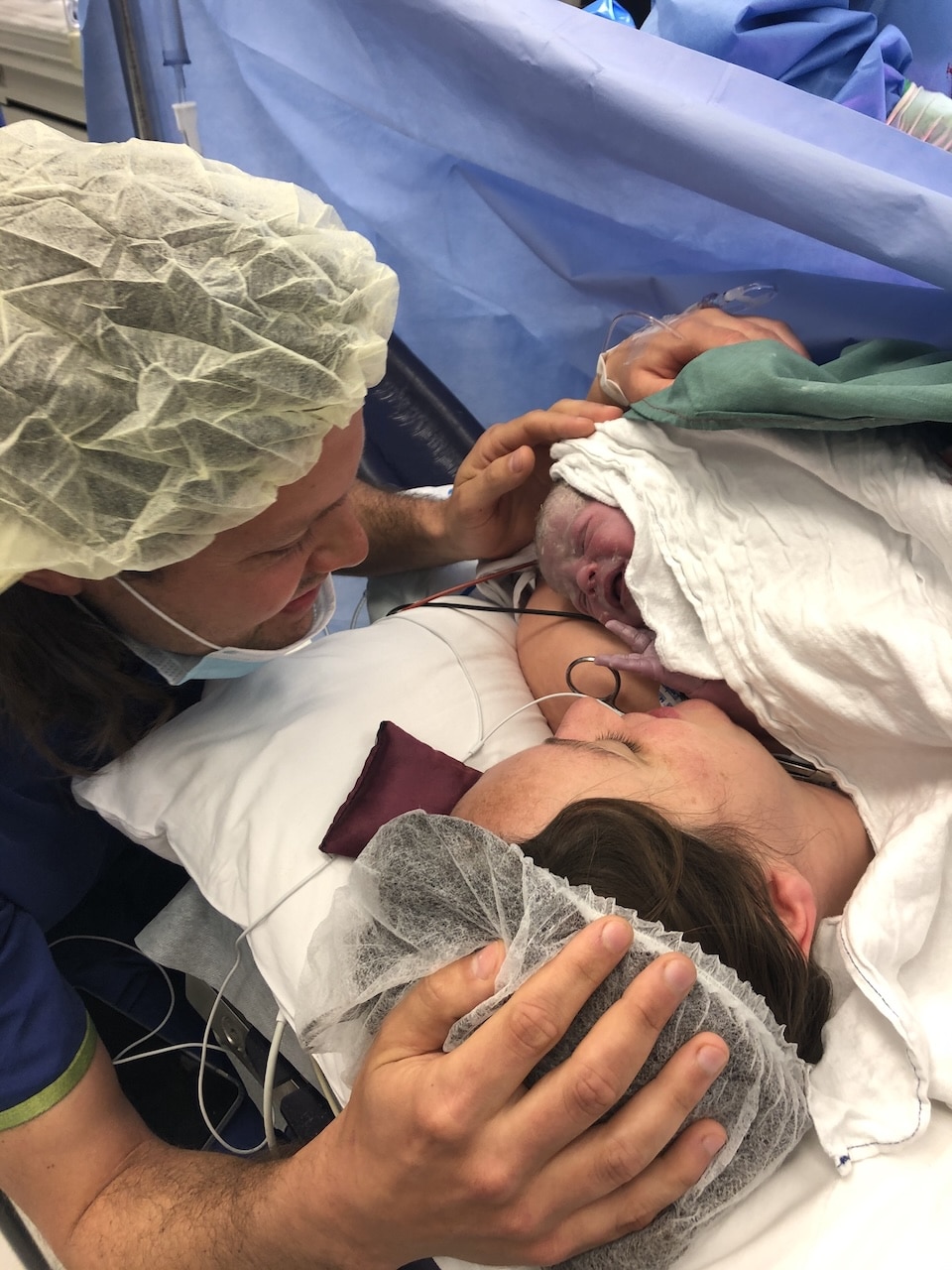
“I was in total denial about how fast it was happening, I got on the bed to start monitoring and the noises I was making started to change…I got wheeled around to the birthing suite and I was fully dilated. I pushed pretty ineffectively for over an hour when the OB was called in as they were wary of my cesarean scar and both mine and baby’s heart rate was high. They told me they needed to take me to the theatre for a forceps delivery but I was determined to stay where I was so I pushed really hard and after two hours they just tried the forceps and her head was born and in the next push I pulled her up onto my chest and it was amazing. She was fine, I cut the cord, she was breathing. It was the best!
“My Postnatal care with my private midwife was amazing because she could check episiotomy, check blood loss as I was a bit concerned about it being heavy. It was nice to debrief…it’s been such a journey to get to this point and I felt really ripped off that I couldn’t sit on the couch with my friends and talk it through. I struggled with the covid restrictions….there’s been lots of crying and feeling overwhelmed and sad at the situation. I just want to be normal, why can’t it be normal!”
When Flick chatted with the community health nurse she said that a lot of new mums had been struggling with similar feelings and it’s called expectational grief; you’re grieving for what you thought your birth and postpartum experience would be like.
“You didn’t expect your midwives to be in full PPE, you didn’t expect not to have your private midwife or any visitors, you’re struggling with not being able to see your friends. It’s compounded by the fact that everyone is struggling, even over the phone, your friends and family are struggling too and they’re probably not as supportive as they could be. Four weeks on and I’m fine and in some ways the isolation has been a hidden blessing. Now that I’m used to it I can see that it has some really wonderful benefits. I’m nowhere near as tired because I’m not running around seeing anyone. It’s certainly not what I wanted but it has been good for me.”



Topics Discussed
Blighted ovum, Covid-19, Emergency caesarean, Induction, Infertility, IVF, Miscarriage, PCOS, Private midwife, Sperm morphology, Vaginal birth after caesarean (VBAC)
Episode Sponsor
Today’s episode is brought to you by Bliss Birth. Bliss Birth is founded on the belief that women’s bodies are incredible things, and that when it’s safe, choosing natural options makes for the best outcomes for mums and babies. That’s why Ariel has developed a range of products to support your natural birth experience. Introducing the most advanced natural pain management device for labour available in Australia – The Elle TENS Plus. TENS stands for Transcutaneous Electrical Nerve Stimulation and it is the ultimate birth tool as it maximizes your body’s natural pain-fighting abilities. For $79 you can hire an Elle TENS through Bliss Birth. The Bliss Birth TENS Hire features; Built in contraction timer, Longer 8 week hire period, Pre-addressed, prepaid return (No printer needed). The ‘Mama Bag’ valued at $10.95 is yours to keep! You can enjoy 10% off Bliss Birth with the code AUSTRALIANBIRTHSTORIES. Head over to BlissBirth.com.au
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us