Podcasts Anna McGahan
EPISODE 169
Anna McGahan

I interviewed Anna about her first birth in episode #61. She talks in detail about her very rare placental abruption at 33 weeks which was only discovered when she stopped feeling foetal movements (primary symptoms are pain and bleeding but Anna had neither). Mercy was born via emergency cesarean and stayed in the NICU for weeks before Anna and husband Jonathan took her home.
After Mercy’s birth, Anna developed intense uterine pain which was almost constant. She was diagnosed with endometriosis, had surgery and two months later, after taking her basal temperature every day and preparing her body for conception, she fell pregnant. She was living in Melbourne at the time and was told by her care provider that her risk of placental abruption had increased to 1 in 10 (it’s usually 1 in 100-200). With this in mind, she was denied midwifery care and went straight to the high-risk category where she saw only OB’s at her local hospital. She admits that a VBAC felt unlikely; her care was very medicalised, there was no discussion or clarity about her opportunities to attempt let alone achieve a VBAC and she felt very unsupported.
After making her way through the first trimester, an experience that was long and often worrisome, Anna was relieved to make it to 12 weeks. However, at 16 weeks she developed visual disturbances where a part of her visual field was erased. After a slew of tests and concerns about a pulmonary embolism, she was diagnosed with pregnancy induced visual migraines that persisted throughout her third trimester.
At 26weeks, after Jonathan received a job offer on the Sunshine Coast, they packed up their Victorian home, made the long trek to Queensland amidst summer bushfires and spent Christmas on the road. In the New Year they arrived at their sweet home, a blue renovated church, and Anna called Sunshine Coast University Hospital with the hopes of booking in with their midwifery team.
A midwife called her soon after and so began a deeply supportive experience that carried Anna through an anxious third trimester and into a healing and joyous birth. “The midwives were spiritual and emotionally engaged and I was really craving that because I experienced it with Mercy. In that first phone call the midwife told me that she was so excited they were seeing me, she told me that I absolutely could have a water birth, a VBAC and yes, Jonathan could stay the night at the hospital. They’re so pro-women and they totally took my circumstances into account but they were never phased by it. I suddenly felt so incredibly empowered.”
Before they moved interstate, Anna and Jonathan attended a hypnobirthing course and she admits that it changed her perspective in so many ways. “The most amazing thing for me was seeing my husband empowered, he saw that he wasn’t pointless, he had a role, he could contribute to the birth experience and my experience. It helped usher him into that headspace,” she says.
The third trimester was particularly difficult for Anna as she worked through the anxiety associated with her trauma from Mercy’s birth. She also switched her perspective and embraced the extra two months of pregnancy that she got to experience, even if her fear of placental abruption was present. “I just kept reminding myself that I get to plan my postpartum, cook for it, plan my birth and get the support I want and need. It was such a gift to get that extra two months. I was able to pour so much energy into manifesting the birth and it helped stave off anxiety I was starting to experience around foetal movement,” she says.
“I wasn’t prepared for the long haul of 40 weeks. Trauma somehow prepares you to expect trauma again. I’m a real advocate for being on top of foetal movements, monitoring and responding to them. Juniper had a pattern of stopping moving; her movement would be fine for a few weeks and then they’d really diminish so I’d go into hospital for monitoring. Hitting 33 weeks was amazing and every week felt like a milestone but I was grappling with doubts about whether I should be more vigilant and whether my body was ideal for this baby.”
At her 36week midwife appointment and after four presentations to the hospital with reduced foetal movement, Anna’s midwife suggested an induction at 38 weeks as multiple presentations could be a red flag. It was difficult for Anna to hear as she desperately wanted a natural birth and she knew the risks associated with induction and cesareans. That said, she strongly believed that she would get the redemptive birth she dreamed of and she felt like an induction was the best choice for her mental health.
She mindfully chose to approach the induction with a positive mindset and treated it as cervical preparation as opposed to intervention. “Everything on the net said that if you have an induction you’re setting yourself up to fail, I’m happy to now provide a positive narrative. I drank lots of raspberry leaf tea, had sex and was very intentional about trying to help my cervix open and be soft and prepared. I was constantly thinking: when I enter this process, it can go really smoothly and my body won’t resist it. I psychologically felt amazing about it, my body felt really amazing and I was ready to go. It was a partnership, I was doing one side and the induction would be doing its work on the medical side. I just took responsibility for my half and treated the syntocinon as my friend and one I was working with.”
Anna and Jonathan went into hospital late in the afternoon so the balloon catheter could be fitted. Usually the hospital doesn’t have restrictions on the amount of people in the birth space but since Covid-19 became serious, they have limited it to one birth partner and that partner must not be showing any symptoms. Anna and Simon settled into a room on the maternity ward yet twenty minutes after the catheter was fitted, she started contracting. “Sometimes they can trigger a few hours of labour’ they were manageable but I had to work through them. My midwife kept coming in, she put clary sage on my acupressure points and I felt so supported. I really thought that perhaps the balloon catheter was all I’d need….but at 3am they just faded. I was crampy but I fell asleep.”
Two hours later she was woken by the midwife and taken to the birthing suite to have her waters broken and the IV hooked up for the syntocin drip. She was hesitant about handing over her birth plan but she needn’t have worried; the midwives were so grateful to know her birth plan and loved knowing what she wanted from her birth experience which included an internal monitor on baby’s head, water birth, delayed cord clamping and placenta encapsulation.
“The beginning stages of labour were so beautiful. The surges came on gently, they were predictable and controlled. There was a simplicity to it; they’d start in the same way and I felt calm. Working through them felt nice, it felt good. When the contractions increased I realised that whatever I was using to counteract the pain was no longer substantial so I would change my position and tactic. Stacey, my midwife, brought a medical student with her and she was like an extra doula. Stacey was really present with us, on board with hypnobirth and active birth and she set up the shower with fairy lights, brought the birth ball in, showed me the positions I needed to get into and started coaching me. She gave 150%!
I got to the point where the pain and fear was overwhelming; I was surrounded by it, I didn’t know how far along I was, I kept saying I was overwhelmed and my midwife encouraged me to surrender to the overwhelm. She said: Everything is perfect, your surges are perfect and she wanted to get me into a more restful situation because there was a degree of panic. Things started to get a bit more spiritual for me and I started asking God for help. I felt a keen sense that it wasn’t going to be much longer but it was going to be hard and I had to embrace that.”
“They put me on the bed and they were trying to get me in a position where I could find a place of calm but I was actually transitioning and I couldn’t stop vomiting. I was bridging two worlds, I couldn’t even speak, words failed me. It was extraordinary, I had this weird feeling that I was transitioning even though no one else realised. I was writhing around and I needed to move my legs, the pain in my back just kept moving lower and lower. I got into childs pose on the bed and my husband started pressing the two points on my sacrum, stretching my body out during contractions and it was the first time in a long time that I was getting relief, and then it was around that point that I felt that twinge in my bum. I had only been labouring for just over three hours at this point, so midwife was preparing for the long haul and she was trying to ease my expectations. She left and I had a surge and my body started involuntarily pushing, it was so intense and satisfying.
She came over and saw the shape of my rectum change and brought a mirror over and then went into midwife mode; she’s putting the bath on, guiding me through surges. I did not expect to be vocal in labour but the bearing down was so primal and guttural that I found myself making the most phenomenal sounds. Roaring, bellowing sounds! The whole experience of pushing is so satisfying, it’s happening to you and through you and I could finally partner with them.
Crowing is the part you build up as being the hardest part but I could feel myself stretching, it wasn’t incredibly painful, but it got to a certain point and she put a warm compress on my perineum, she felt me internally tear and she asked me to turn on my back, and she told me she’s not one to make a decision like this but she chose to take action as she was worried that I’d torn through to my rectum, I trusted her and I was comfortable with that level of intervention.
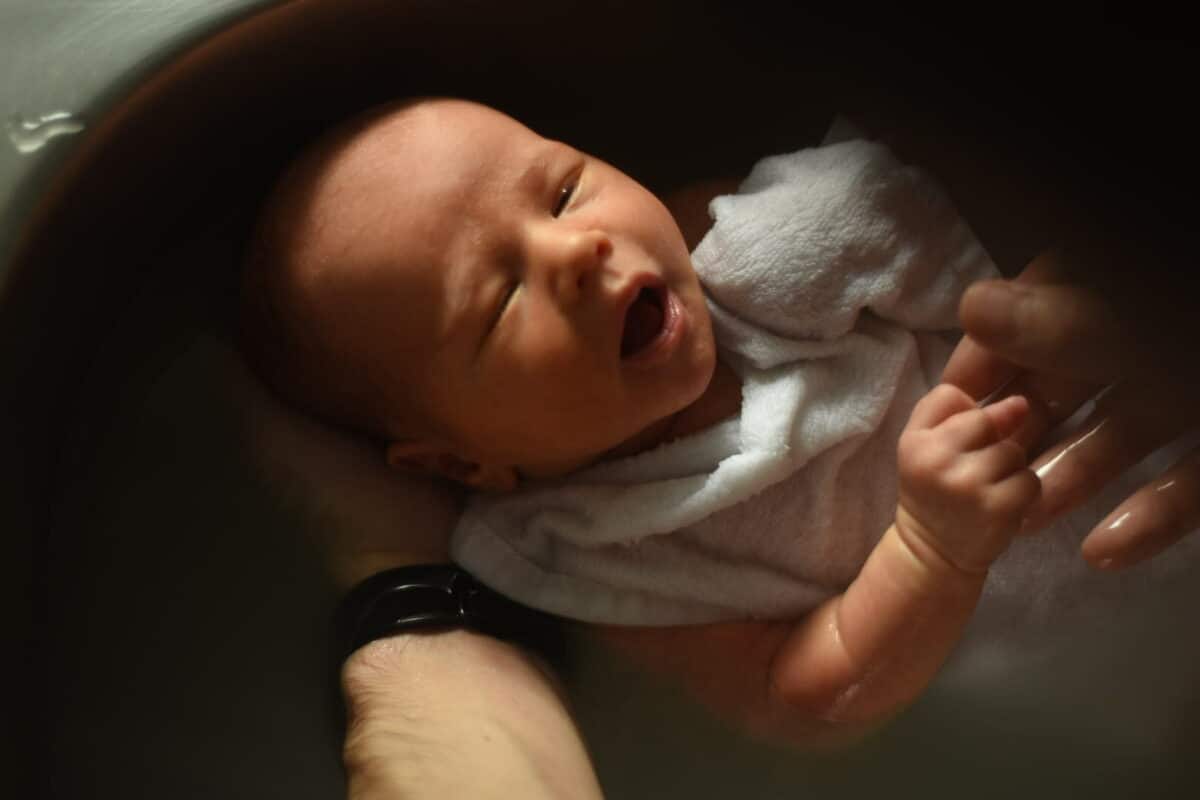
I leant forward and pulled Juniper up and I had imagined that moment so many times, I’d longed for that moment, grabbing my baby and putting her on my chest, the healing of that was one of the most important things that I wanted, to have this tiny baby on my chest, it was the most satisfying experience of my life.”
Anna was offered a 6-hour discharge but was in no way forced to take it. It’s a precautionary step offered to every patient since Covid-19 started in the hope that it reduces the risk of infection. Anna chose to stay overnight and went home the following morning. She says that even though she birthed in the midst of the pandemic, the midwives were still hands on, engaged and involved.
She also noted that the midwifery staff were secretly happy about the no visitors rule. “They were actually noticing better breastfeeding rates, calmer mothers and better mother and baby outcomes because they didn’t have the stress and exhaustion of visitors twice a day.”
“I’m not going to lie, there was such a deep relief in knowing that no one can visit and no one is expecting me to leave the house. I can just be here, it’s actually exactly what we need. That said, the support on the other side of birth is pretty minimal compared to what it usually would be. Which is easier if you’re a second or third time mum, but tricky for first time mums.”
A midwife visited Anna on her second day home from hospital and she went to her GP at the end of the first week but apart from that, she’s had very little care.
She offers this advice to mothers preparing to birth in a Covid-19 world:
“We prepared all our meals in advance so we weren’t relying on meals from other people and the strangeness of knowing we weren’t going to get physical support meant we had to reposition our minds and expectations. There’s massive pros (you can actually experience the beautiful confinement period which is just about family bonding), but at the same time you have to ask yourself: how do I counter the stay at home loneliness of being a mum with a newborn? How do I set up my friendship network so I don’t feel isolated?
We’re going to have to figure it out as we go along. This is the time to really appreciate the comfort of online friendships, there’s something so powerful about the circle of mothers, we’re the secret superheroes in this current climate, we need each other more than ever.”




Topics Discussed
Covid-19, Hypnobirth, Midwifery care, NICU, Placental abruption, Positive induction, Vaginal birth after caesarean (VBAC)
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us






