Podcasts Roisin – miscarriage, IVF, HG, MGP, gestational hypertension, preeclampsia, induction, emergency caesarean, MCDA twins
EPISODE 499
Roisin – miscarriage, IVF, HG, MGP, gestational hypertension, preeclampsia, induction, emergency caesarean, MCDA twins

When she found out she was pregnant with identical twin girls, she was referred to the maternal foetal medicine team and remained under their care for her whole pregnancy. Despite an early labour scare at 32 weeks, Roisin continued on with life at home and it was only when she went to hospital a little concerned about one baby’s movements, that she discovered she was in active labour. Her twin girls were born an hour later and she explains in detail the anguish of NICU and her determination to breastfeed, despite the hurdles of triple feeding.
“Both my pregnancies were IVF. We tried for a year to conceive and I’m a type A personality so considering we were both 25 and healthy, I wanted to get investigative procedures done, especially because I conceived a few times and had a few early miscarriages. This revealed a factor of male infertility and a progesterone deficiency for me. On my first egg collection I got 15 eggs and we ended up with five embryos. I’d worked with a nutritionist for supplementation and I did acupuncture and I think that contributed to a great egg collection. I went through hyperstimulation so I couldn’t do a fresh transfer and that was heartbreaking.
“We did a frozen transfer the next month and I conceived but I lost that pregnancy as well. For the next transfer I increased my progesterone dose and that was my son; I stayed on progesterone till 16 weeks. One box of 15 pessaries is over $100 so it’s very pricey. The joy of seeing a positive pregnancy test was gone and I felt like I needed to just focus on the next step. I feel like I was anxious till he was born and crying.
“I had hyperemesis gravidarum and I was working an office job and vomiting countless time a day. I took medication which stopped the vomiting which was great but it didn’t help with the nausea; that lasted about 24 weeks. I had 10 weeks of a second-trimester glow and aside from the anxiety, I really enjoyed being pregnant. I knew I wanted to do Midwifery Group Practice (MGP) in the public system and I loved my experience. My goal with Finley’s birth was an unmedicated vaginal birth and my midwives really helped me prepare for that.
“At 34 weeks I went to my appointment and I’d had pretty severe headaches for three days. My midwife was concerned and she asked me to come in the following day for urine and blood tests. My blood pressure was also igh so they encouraged me to get a blood pressure machine from the chemist so I could monitor it at home. I started getting blurred vision and that was incredibly concerning. At the time my urine and blood results were normal so I was diagnosed with gestational hypertension. When it became preeclampsia, it felt like a systemic illness; I felt like a very sick person. When I was officially diagnosed they told me I’d need an induction at 38 weeks and I knew the risks of a pregnancy with preeclampsia but I also knew an induction was the fastest ticket to a birth experience I didn’t want.
“I was admitted to hospital and had the foley balloon inserted. At 11pm it fell out and I got quite excited but nothing happened overnight. The next morning I tried to push out the syntocinon but I couldn’t because it was an induction for medical reasons. The contractions were coming every minute and I used all the techniques – the comb and the TENS machine – but it was tough. I had been labouring for seven hours when my midwife asked if I wanted a vaginal examination because I wasn’t really coping. I was about 2-3 cm and that shook me.
“At about 4pm I asked for the epidural which was difficult for me. Unfortunately it failed which was such a shame because I was bedridden – I had heaviness in my legs but there was no pain relief. The second time it went unilateral so half of me was number, but I could feel the other side. I’d been labouring for close to 16 hours when they checked me again and I was still 3cm. Luckily I’d done so much birth education and I knew that a caesarean birth was likely with my diagnoses and a necessary induction. It was a category two emergency caesarean because Finley’s heart rate was decelerating. The room flooded ith people but everyone was calm and explained everything to me. Finley was born and he cried and it was such a relief.
“The thing I hadn’t thought about was the stitching up afterwards. I started getting feeling back when they were repairing me. I had heaps of milk which I was thankful for and so when I was back on the ward, I asked every midwife for guidance and assistance. We were discharged after two days and had an amazing postpartum. I breastfed him till 13 months.
“The number one thing I felt about my birth was, I was informed I definitely consider that I have birth trauma but I feel like it would have been far, far worse if I didn’t have the education, information and awareness I did. In a debrief with the OB, he told me that I have an extra long scar on my uterus so a VBAC was unlikely in the future. That was the hardest part of Finley’s birth; knowing that my experience was going to inform all future births.
“Finley turned one and we started IVF again and I fell pregnant. We went on a family holiday and I did a pregnancy test and the line was incredibly faint. That miscarriage hit me really hard. I bled naturally so I didn’t have to have a medically induced miscarriage; my body did what it needed to do. On the next transfer, they transferred one embryo and it split, and I’ve got identical twin girls. They’re MCDA twins; two sacs, one placenta. My hyperemesis was markedly worse; I couldn’t be upright and that’s when I said to my husband as a joke that it might be twins.
“I can’t explain the moment when we found out we were having twins; excitement, shock and fear all in one. They couldn’t see a membrane between the babies at that stage so they were concerned it was the most high-risk form of twin pregnancy and they basically said, don’t get your hopes too high until the 12 week scan which is not what anyone wants to hear, let alone someone with a long history of miscarriage. We went to an additional scan and they could see the membrane which was great, although it was still considered high risk because they shared the same placenta.
“I was in the tertiary level of care under the maternal foetal medicine team. I was scanned every two weeks which was a very different experience to my first. They were beautifully behaved in there; it was a textbook pregnancy and they stayed almost the same size throughout the whole pregnancy. A twin pregnancy is uncomfortable but after about 26 weeks when HG eased, I loved being pregnant. I was advised to stop working at 32 weeks because I would be having them at 36 weeks, if I made it that far. I finished work on the Friday and the next day I packed my hospital bag. By about 3pm I’d noticed that I was having consistent cramps; they were coming four times in 10 minutes. I went to hospital – with my handbag and kindle presuming I’d be home that night. I was 32+2 and the contractions were on. The pain was manageable because it wasn’t an induced labour. They did a cervical check and I was only 1 cm dilated but considering I had a high risk pregnancy, they admitted me and I needed to have the steroid injections for their lungs. I was shocked by the fact that I was about to have premature babies.
“The team kept reminding me that it could turn into active labour at any point. I was in hospital for about 11 days and my mental health was really affected. I had a discussion with the nurses and told them I really needed to weigh up the pros and cons. The plan was, if anything changed, I needed to come immediately to hospital. I’d had the symptoms for so long, I knew I’d notice a change. When I was discharged, the contractions really settled and slowed.
“Every morning I wore up and was still pregnant, I was grateful. At 35+4 I went to bed and noticed that twin B was a bit quieter. Stupidly I went to bed and that was the wrong decision. I felt her move but it was so much less and I had an intuitive sense that it wasn’t right. At about 10am I went to the hospital for a check-up; the baby’s heart rates looked really good but they also noticed that Twin B wasn’t moving much. The obstetrician brought in the bedside ultrasound monitor and Twin B wasn’t as responsive as we’d expected so she went to talk to the maternal foetal medicine team. She asked my consent to do a quick cervical exam and she looked at the midwife and I knew straight away. I was 4 cm, my waters were bulging and I was in active labour. All of a sudden I was being prepped for an emergency caesarean.
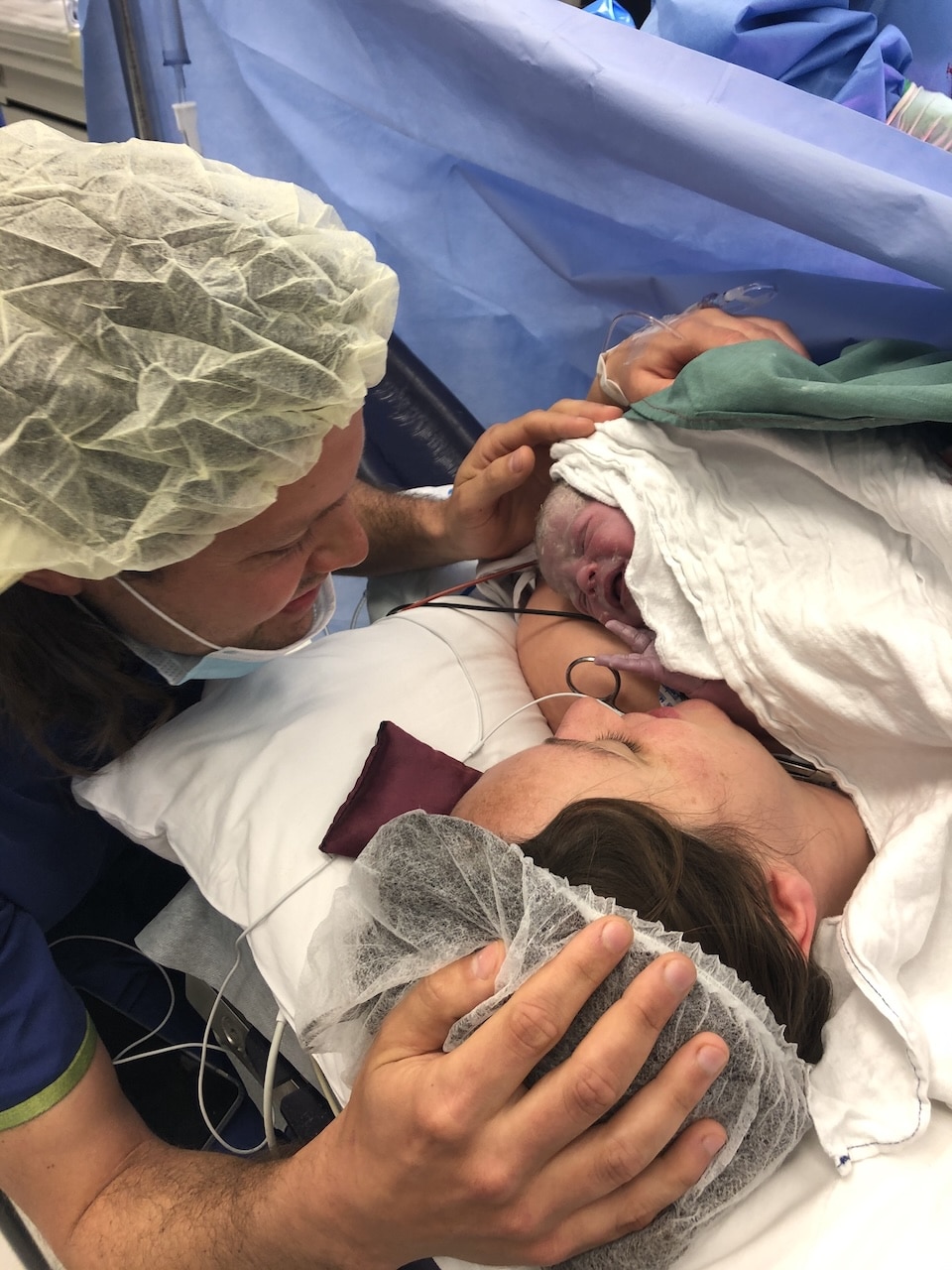
“My husband made it just in time. Both girls were born crying but they went straight to the neonatologist team – there were two teams in the room. I was really prepared for how busy the room would be and I’d consented to have medical students present to watch and learn. I appreciated how calm everyone was. Odette was whisked away straightaway to NICU but Murphy came to me for a short time before she had to go to NICU for breathing support, too.
“I went back to the ward by myself so I did what I knew I could do, express colostrum. The midwives came in and helped me express and I had a really good supply; my body knew what to do. The babies didn’t need any form of supplementation and I was really proud of that.”




Topics Discussed
Emergency caesarean, Gestational hypertension, HG, Induction, IVF, MCDA Twins, MGP, Miscarriage, Preeclampsia, Three babies
Episode Sponsor
Today’s episode of the show is brought to you by my online childbirth education course, The Birth Class.
What makes The Birth Class so unique?
Well, instead of learning from one person with one perspective, we’ve gathered nine perinatal health specialists to take you through everything you need to know about labor and birth.
Realistic information is key to thorough preparation.
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us