Podcasts Maddie – Homebirth, private midwife, cleft lip and palate diagnosis, exclusive pumping journey
EPISODE 578
Maddie – Homebirth, private midwife, cleft lip and palate diagnosis, exclusive pumping journey

Maddie’s Preconception Journey and Early Pregnancy
Maddie’s path to motherhood began with thoughtful preparation after she and her fiancé Mark chose to prioritise starting a family over wedding planning. “I’d been vegetarian for 12 years and I just wanted to check out how my health was in that sort of space for having a baby nutritionally,” Maddie explains. Her proactive approach included working with a nutritionist, having blood work done, and receiving an iron infusion to optimise her iron stores for pregnancy.
After weaning off antidepressants with psychiatric support and focusing on lifestyle improvements for several months, Maddie conceived on their third cycle of trying. “For the first time that we got a negative test, I was absolutely devastated. I, even though I knew that it could take a while, it really, I just thought, oh, I’ve done all the right things and it should, isn’t that how it works?” she reflects on the emotional rollercoaster of trying to conceive.
Choosing Home Birth and Midwifery Care
Long before meeting her partner, Maddie had been passionate about physiological birth. “Even before I met my partner, I’d followed different accounts and read certain books that really made me quite passionate about having a home birth,” she shares. After eight years together, she and Mark had thoroughly discussed their birth preferences, leading them to interview Mama Toto midwives months before conceiving.
Maddie’s first trimester brought significant morning sickness: “I was vomiting from about six weeks to maybe about 16 weeks maybe. Four or five times a day. But it came on very quickly and then I’d be sick and then I could get on with my day.” Remarkably, she continued experiencing daily morning sickness right until birth, though it became more manageable after 16 weeks.
The 22-Week Scan: Receiving the Cleft Diagnosis
What should have been an exciting 20-week scan (delayed to 22 weeks due to Christmas timing) became a life-changing moment. “I hadn’t really, maybe a bit naively, I hadn’t really thought too much more about the scan. So when we were in there… I felt that she was checking his face for a lot longer,” Maddie recalls.
The sonographer’s words – “I can see that your baby has a cleft lip and I think a cleft palate” – sent Maddie’s world spinning. “At that moment it really took me off guard and I think I just said, oh, okay. And I didn’t really process that until she left the room and, yeah, it fell apart pretty quickly.”
The following weeks were emotionally challenging as they waited for confirmation. “I just stayed in bed and cried for about four days,” Maddie admits. “I just really felt all of a sudden, I cared for so many other people’s children and so many other babies. And now it was my turn and it just felt so unfair.”
Navigating Hospital Systems and Maintaining Home Birth Plans
The cleft diagnosis introduced complex medical considerations whilst Maddie fought to maintain her home birth plans. Her midwives remained supportive: “It was never a hard no from them. It was what everyone was comfortable doing and what they were comfortable with.”
However, navigating backup hospital arrangements proved frustrating. Monash Hospital, where they were receiving cleft care, refused their transfer referral. “I think the obstetric team didn’t think that home birthing was an appropriate decision and weren’t going to accept us as a backup referral,” Maddie explains. This meant potentially transferring to Frankston Hospital during labour, then moving to Monash postnatally – a logistically challenging situation.
Preparing for Feeding Challenges
Learning that traditional breastfeeding wouldn’t be possible was particularly difficult for Maddie. “That was, yeah, another. And like I said, it’s still a bit of a challenge at times now, like a real grief for me. I just wanted to home birth my baby and, carry them in a carrier and breastfeed wherever I wanted. That was my dream.”
The cleft team provided education on specialist bottles and feeding techniques. Maddie also connected with Tracy Davey, an IBCLC with cleft experience, to prepare for exclusive pumping. “I was able to collect colostrum prior to birth too. So we knew that in the first few days we would do what’s called finger feeding.”
Waters Breaking and the Waiting Game
At 38+2 weeks, after losing her mucus plug and experiencing period-like cramping, Maddie’s waters broke during the night. “I went to the toilet and then I stood up and I was like, more liquid came out. I was like, well, that’s not wee. And it was like a little bit pink and I was like, I think that’s it.”
What followed was an anxious 72-hour period of monitoring and waiting for labour to establish. “During the day I continued to be a little bit crampy. But they did peter out during the day,” she describes. The midwives’ approach was supportive: “The parameters around when your waters break with our midwives were, we wanted to watch all other aspects of my health, baby’s health. So there wasn’t a, it wasn’t automatically an emergent situation.”
Hospital Monitoring and Maintaining Autonomy
Maddie chose to have monitoring done at Solas Health in North Melbourne rather than Frankston Hospital to avoid pressure for induction. “My midwife said, you can go to Frankston, or there was a place… where they can do the same monitoring… But there’s no what’s the word? No judgement, no discussions. It’s just you come in for your appointment and you’re on your merry way, which sounded lovely to me.”
When reduced fetal movements necessitated monitoring at Frankston, Maddie felt the familiar anxiety of being in a hospital setting. “I really hated being there. I was quite emotional, the fact that we were going in there at all… I started to feel, this is not the pregnancy that I’d hoped for. This is not the baby I’d envisioned. And it started to really feel like the home birth was gonna be taken from me too.”
Labour Begins: The Power of Trust and Support
After a stretch and sweep at 72 hours post-rupture, labour finally established. “I think I would’ve been on all fours, really bracing into the couch, moaning for maybe a good 20 minutes with no tens, nothing just, which in hindsight, I probably should have put the tens back on, but I thought it would cool down faster.”
Maddie’s labour was intense and rapid once established. “It went from that two o’clock when I felt things this spicy. It just, it was like that until he was born. I really didn’t have much of a lead up at all.” Her experience of transition was particularly challenging: “I really started to think, so am I gonna get to the hospital to get pain relief? Like, I can’t do this until 11:00 AM thinking that’s when my baby would be coming, hours to go.
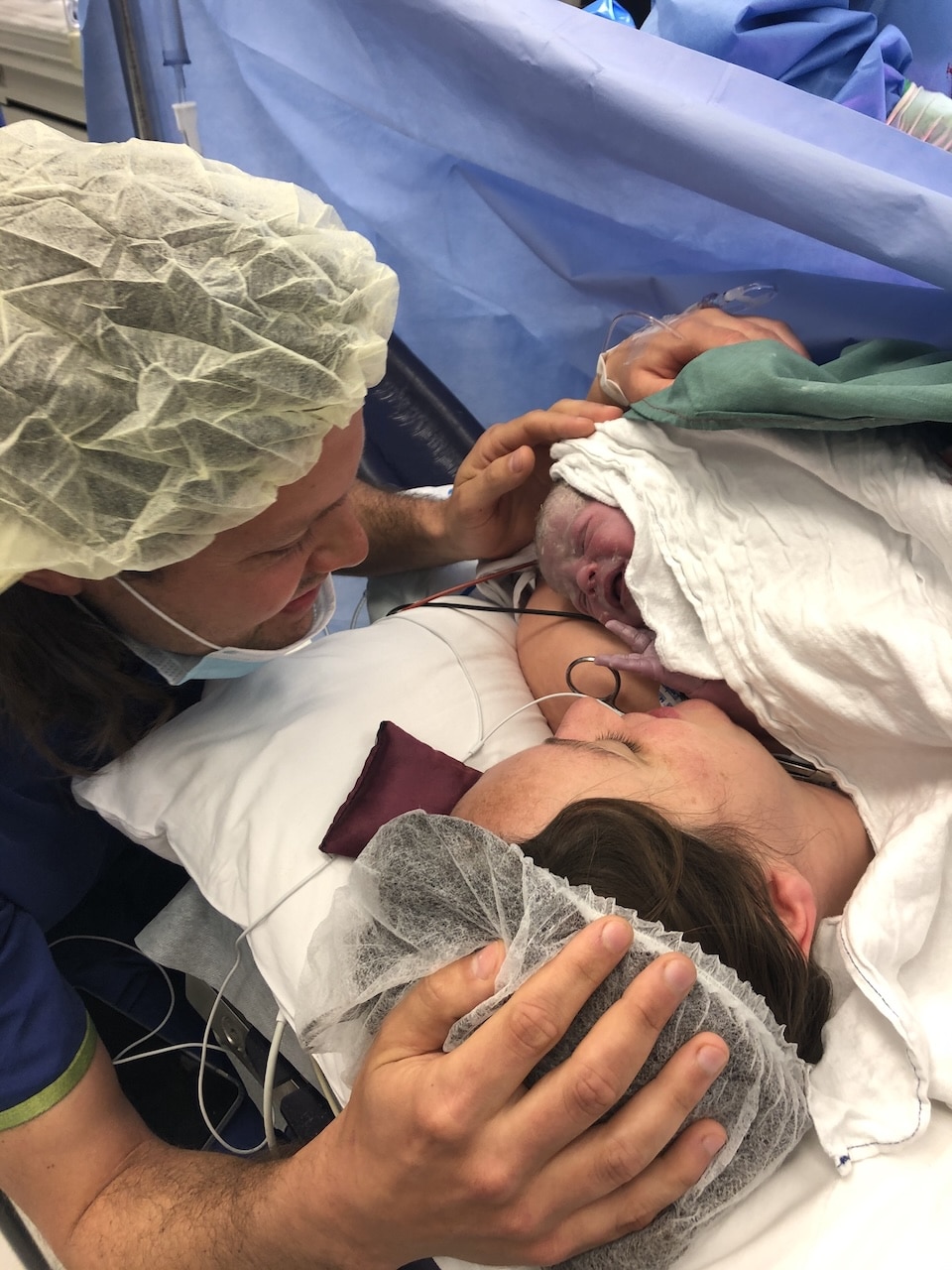
Despite the challenges, Maddie achieved her desired water birth at home. “I stayed in the pool with Freddy for about half an hour, and they kept topping up the warm water and I just held him and marveled at his beautiful baby, this beautiful baby in my arms.”
The moment of birth was profound: “It was like, all of that was just melting away. I just felt like, I did it, all these things that I thought I wasn’t, I wasn’t having the way I wanted, but we got to birth the way we wanted.”
Meeting Baby Freddy and Early Feeding
Freddy’s arrival brought relief and joy. “He had a little cry, not a massive cry. It took a little while to do some clearing and so, yeah, we were watching that at first, just to be sure, that he was okay and he was, and then eventually, yeah, we got a few more big cries.”
Maddie was able to attempt a breast crawl and comfort latching, which her IBCLC had encouraged. “She actually said that there’s no reason that I couldn’t try to latch him for comfort, and there’s still so much benefit in supporting that. So, I was able to do that, which was really lovely and emotional.”
Postpartum Challenges and Ongoing Journey
Freddy’s feeding journey required specialist bottles and exclusive pumping, but he adapted well. A hearing test revealed mild to moderate hearing loss – common with cleft palate – requiring a hearing aid headband. “The first time we put that on we could really tell that he hadn’t really been hearing us. So it was really lovely just to say hello to him and his face just lit up.”
The surgical journey ahead includes lip repair at six months and palate repair at one year, with potential additional procedures as Freddy grows. “We certainly know that the path for cleft babies and their surgeries, it’s not it’s not a short path.”
Reflections on Resources and Support
Maddie’s experience highlighted the lack of Australian resources for families facing cleft diagnoses. “Cleft diagnoses are one in 700 and I’m pretty sure… Down Syndrome is one in a thousand… it just really at the time, made me feel where are all the resources? Where’s all the other parents?”
Her story powerfully demonstrates that with the right support team, informed decision-making, and trust in the birth process, it’s possible to achieve a positive birth experience even when facing unexpected challenges. As Maddie reflects: “I couldn’t believe for years, prior to meeting my partner, I knew I wanted a home birth, and here I was and I did it.”
Key Takeaways for Expectant Parents:
- Thorough preconception health optimisation can support a healthy pregnancy
- Unexpected diagnoses don’t automatically preclude physiological birth choices
- Building a supportive care team is crucial when facing additional challenges
- Hospital policies may not accommodate individual circumstances – advocacy is important
- Exclusive pumping can be a successful feeding method with proper support
- Early intervention and specialist care significantly improve outcomes for babies with cleft conditions
This episode offers hope and practical insights for any family navigating pregnancy with additional considerations while maintaining their birth preferences.


Topics Discussed
cleft lip and palate diagnosis, exclusive pumping journey, homebirth, Private midwife
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us