Podcasts Sophie – premature birth, NICU, tube-feeding, triple-feeding, mastitis, exclusive breastfeeding
EPISODE 493
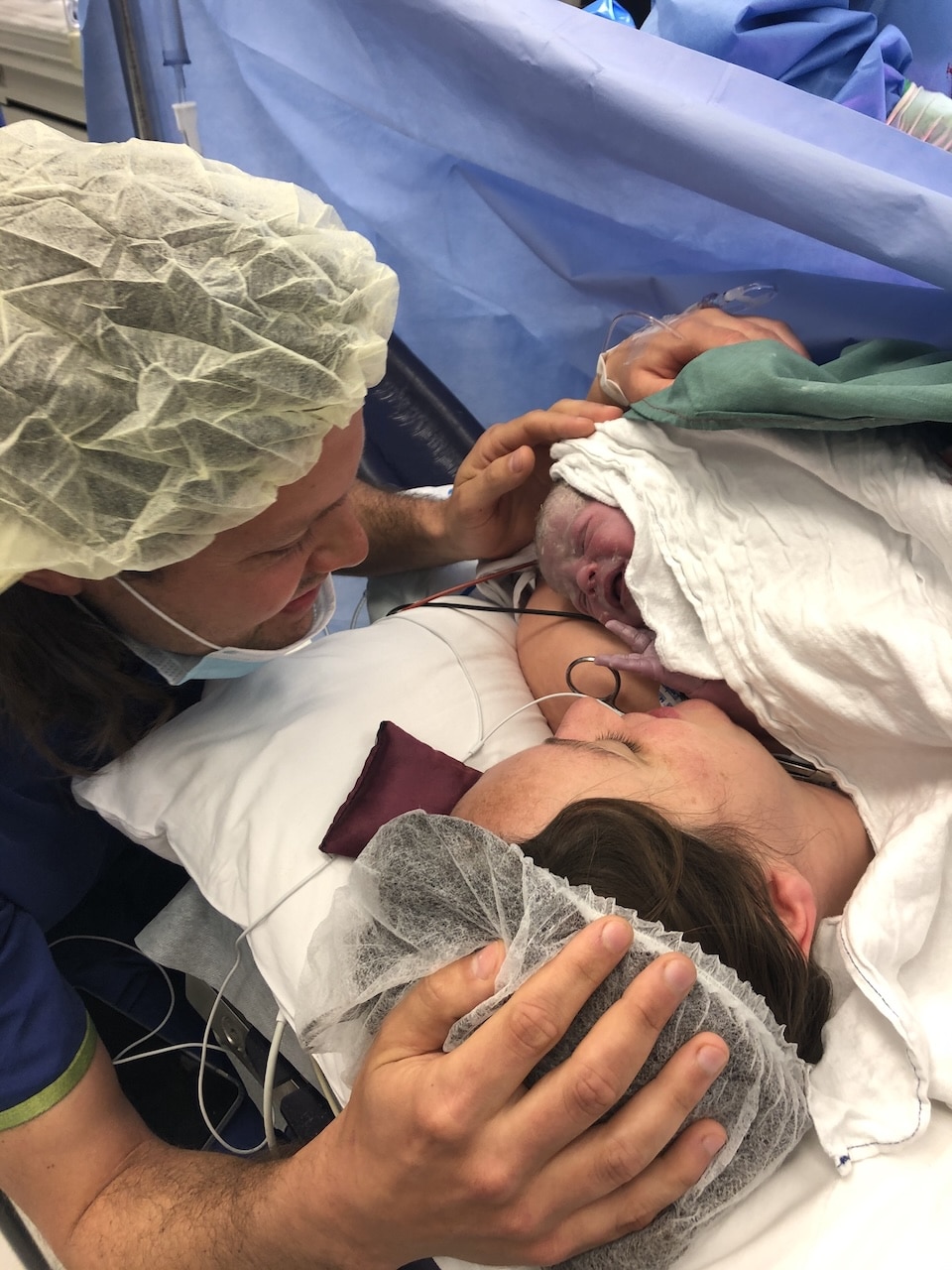
Sophie – premature birth, NICU, tube-feeding, triple-feeding, mastitis, exclusive breastfeeding

Just a note, Sophie also discusses her experience with mastitis and the extra pumping and feeding she did to recover. Advice regarding mastitis treatment has changed in recent years and extra pumping and feeding is no longer recommended as it contributes to inflammation.
“We had an interesting start to Tllie’s life; she was born preemie at 29+4 weeks and was only 534 grams. An amniotic band was found on my 20 week scan and at the 25 scan to check on it we found out the placenta was insufficient and she had stopped growing at 22 weeks. We were told that she wouldn’t survive but we made it to 28 weeks and she was 500 grams which was the baseline for survival so from there it was full-steam ahead or termination for medical reasons (TFMR). The NICU and breastfeeding journey was the easy part compared to the waiting in pregnancy to see if she’d survive.
“She was tube-fed right up until her due date. I had a caesarean birth and so I felt like I had to really work at getting colostrum and to top it all off, I had covid so I couldn’t see her for eight days. Getting my milk in was a really big challenge and so difficult being in hospital in isolation. I had a fairy godmother of a midwife who would sit with me and encourage me and help me with pumping.
“We introduced breastfeeding at 35 weeks. You really have to advocate for yourself in NICU, especially when it comes to maternal, enjoyable things because breastfeeding at that stage wasn’t life-sustaining for her. I was really focussed on giving her a dummy after tube-feeding so she would associated sucking with being full and I introduced an ISOC which is a q-tip dipped in breastmilk so when she was being tube-fed she also experienced the taste of the milk in her mouth. It gave me a sense of control; it was the one thing I could do – pump and give her the ISOC when she was tube-feeding.
“I introduced the nipple at every tube feed that she was awake for and at 37 weeks they switched the tube from down her mouth to down her nose. She was medically stable most of the time; it was just her size that was the concern. The staff told me that one day she’d just get it and she did but because she was so tiny and sleepy, weight gain was our biggest challenge. I was lucky with supply; I had oversupply if anything, I had a freezer-full of milk.
“When the tube came out we were doing alternate breast and bottle feeds and offering a bottle top-up after every feed. Once we were discharged she was on three-hourly feeds but we went to feeding on demand which was roughly 2-3 hours. I had so much milk in the freezer so I didn’t have the stress of low supply; I could have a bottle set-up ready to go,I’d breast or bottle feed her, give her to Ben or whoever was visiting and then I’d pump and freeze that. I did that every 2-3 hours around the clock and I really focussed on bottle feeding overnight.
“For five months after being discharged, we had to have weekly and then fortnightly weigh-ins. It’s hard not to be consumed by it and although we’d have bad weeks, the curve was always trending in the right direction. There was a lot of appointment burden early on which is the experience of all preemie babies. I would try and get to appointments and try to time feeding and pumping and having fresh milk that’s warm…I wouldn’t wish it upon anybody but of course it’s worth it.
“We got to the point of exclusively breastfeeding when she was 5kg, which was five months after she got home. I never considered not breastfeeding. In NICU seeing other babies coming through, the feeding preferences from all the doctors was breastmilk because it’s more suited to the babies underdeveloped digestive system so they would use the mother’s milk and if she didn’t have enough that’s when they would use donated milk. I always just presumed I’d breastfeed but I never realised how challenging it could be. I would 1000 percent triple-feed again to make sure I could breastfeed.”

Topics Discussed
exclusive breastfeeding, Mastitis, NICU, Premature birth, triple-feeding, tube-feeding
Episode Sponsor
Medela has worked with generations of mothers to create innovative breast pumps that are practical and intuitive.
Their Freestyle Hands-Free Breast Pump is a game-changer for postpartum because it gives mothers some fantastic options they have not had before. The benefits are impressive. The ultra light-weight collection cups are designed to sit discreetly in-side your bra. There’s no fuss and it’s easy to clean and assemble with 3 dishwasher safe parts. The transparent design makes it easy to align your nipple and ensure the milk is flowing. For a superior hands-free pumping experience, The Freestyle Hands-Free Breast Pump is recommended for its simplicity and ease of use.
Medela blends decades of scientific research with insights from mothers to create practical pumps that lighten the load – quite literally – in early motherhood. Medela – the Science of Care.
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us