Podcasts Amelia – twins, PROM, emergency caesarean, twin VBAC, breastfeeding, Dr Bisits, breech vaginal birth
EPISODE 487
Amelia – twins, PROM, emergency caesarean, twin VBAC, breastfeeding, Dr Bisits, breech vaginal birth

“I’d dreamt about having kids since I was young. We fell pregnant within a few months of trying. I’d been listening to the podcast for quite a few years and I’m a paramedic so I’d attended a few births on the road. One of the things I’d learnt was that I really wanted to be in MGP so I knew to call early. As soon as I found out I was pregnant I went to my GP for a referral.
“I went in a bit naive, having witnessed very quick labours where women have birthed unplanned at home or in the back of an ambulance so I thought I’d just go with it. Second time around I definitely prioritised birth education. I had a threatened preterm labour at 25 weeks but thankfully that eased on its own. I was on progesterone tablets from then on and presumed I’d go into spontaneous labour but I didn’t. Because I had that mindset, I felt like I was overdue at 39 weeks which became a real mindgame. I got tense and didn’t trust that my body would do it. I had two stretch and sweeps and at 40+3 my waters broke in the middle of the night. There was a dark tinge to the waters which my midwife told me was meconium so I went to hospital straight away to get induced.
“After a few hours, once the drip had been turned up, the contractions were back to back and I was frightened because I didn’t get a break. I got in the bath and tried the gas but it was pretty tough. I laboured for about three hours before I requested an epidural. I got out of the bath and they checked me and I was already eight hours. They encouraged me to keep going because I was so close and likely in transition. I was hopeful at that moment but they also noticed that I was involuntarily pushing which is common with posterior babies. I laboured for another two hours but I wasn’t progressing and Hugh’s heart rate was starting to drop with the contractions.
“I requested an epidural but it took an hour for an anaesthetist to come. As soon as it was administered my blood pressure dropped and Hugh’s heart rate did, too. After about five minutes the atmosphere in the room changed and all of a sudden the room flooded with people. I was told that I’d need a general anaesthetic because the epidural wouldn’t work soon enough. I had to sign a consent form and at that moment I really thought I’d wake up and not have a baby. I knew it was an emergency because they were working really quickly and they were flustered.
“We got to the theatre and they checked me and I was 10 cm and his heartrate had stabilised so the plan changed again. They could see that his head was swollen, too and that would make an instrumental birth difficult. I asked for a few minutes to make a decision. I was so exhausted and afraid so I consented to a caesarean birth. I was gutted because I was fully dilated and ready to go. My husband was absolutely distraught and when I asked him later what was going through his mind, he thought he was going to lose both of us.
“Hugh was absolutely fine but they didn’t lower the curtain so I couldn’t see him. I was so grateful to hold him. My recovery was hard; I had a uterine tear, retained placenta and a PPH. I had a lot of help with breastfeeding in the hospital and when I got home I just remembered the disappointment. I kept wondering ‘what if’ and being given the choice and having the decision on my shoulders…I struggled to know if I’d made the right decision. It took a good couple of weeks to heal and come to terms with everything. My midwife visited us a few times over the first few weeks and it was very sad when she discharged me from her care.
“We started trying for another pregnancy when Hugh was seven months old and then we fell pregnant the week of his first birthday. I knew I wanted a VBAC so I accessed MGP early but that all changed at the first scan when I found out I was having twins. I was convinced there were two babies because I had implantation pain and bleeding three days apart. It was such a bizarre feeling but it was such a deep knowing. My local hospital wasn’t supportive of a VBAC with twins so I called all the private obstetricians and they all said no. I messaged Hazel Keedle on instagram for her advice because I wanted to be with a care provider who would be supportive throughout the whole pregnancy. She recommended the VBAC support facebook group and it was amazing how many people had had successful twin VBAC. My doula suggested I contact Dr Bissits at the Royal Hospital for Women. We were out of the area but the day after I inquired the receptionist called me and Dr Bissits said he’d help me. His approach was so beautiful, he was so reassuring and supportive.
“I managed to get on the MGP programme – we were the first twin pregnancy for them and now they’re regularly taking twin mums. I really felt that a VBAC was possible but that we’d also be safe. I knew if at any stage Dr Bissits turned to eb and said ‘now is the time for a c-section’ I wholeheartedly trusted his knowledge and opinion.
“At 32 weeks we moved from Sydney to the Central Coast. At 34+5 I started to feel a big shift in my body. For context I’m only 4ft11 and I felt such immense pressure; I’d been measuring full term since 32 weeks. Sure enough I woke up the next morning and my waters broke. We drove to Sydney and they confirmed it was my amniotic fluid and they were happy to watch and wait. I started the oral antibiotics but they were concerned about our distance from the hospital so they wanted to admit me. We chose to stay in a hotel that night, we drove back to the Central Coast to get Hugh and we had a telehealth call with Dr Bissits about the birth plan. I started to have irregular contractions so we took Hugh to his grandparents on the Northern Beaches. I put Hugh to bed, had a shower and told the babies they could come and sure enough, labour went from zero to a hundred.
“I called my midwife and told her we were coming in and by the time I got there I was having three contractions in ten minutes. The CTG monitoring was really challenging throughout the whole labour – we kept losing the trace on twin B. I laboured for six hours and then I decided to have an epidural – it’s what I felt like I needed to do. I could still feel when the contractions were coming but the epidural also slowed them down. As soon as I had the epidural everything changed; all the lights went on and they were so concerned with monitoring that I just said no more. Dr Bisits came in and I expressed that I was happy to accept intermittent dopplers every 15 minutes and in the meantime, can you give me thirty minutes without interference from anyone. They gave us that – everyone left the room and we put on music and had a chat and a laugh. When they came back I was fully dilated and I was so proud that I’d advocate for what I needed – uninterrupted time to be in the birth space.
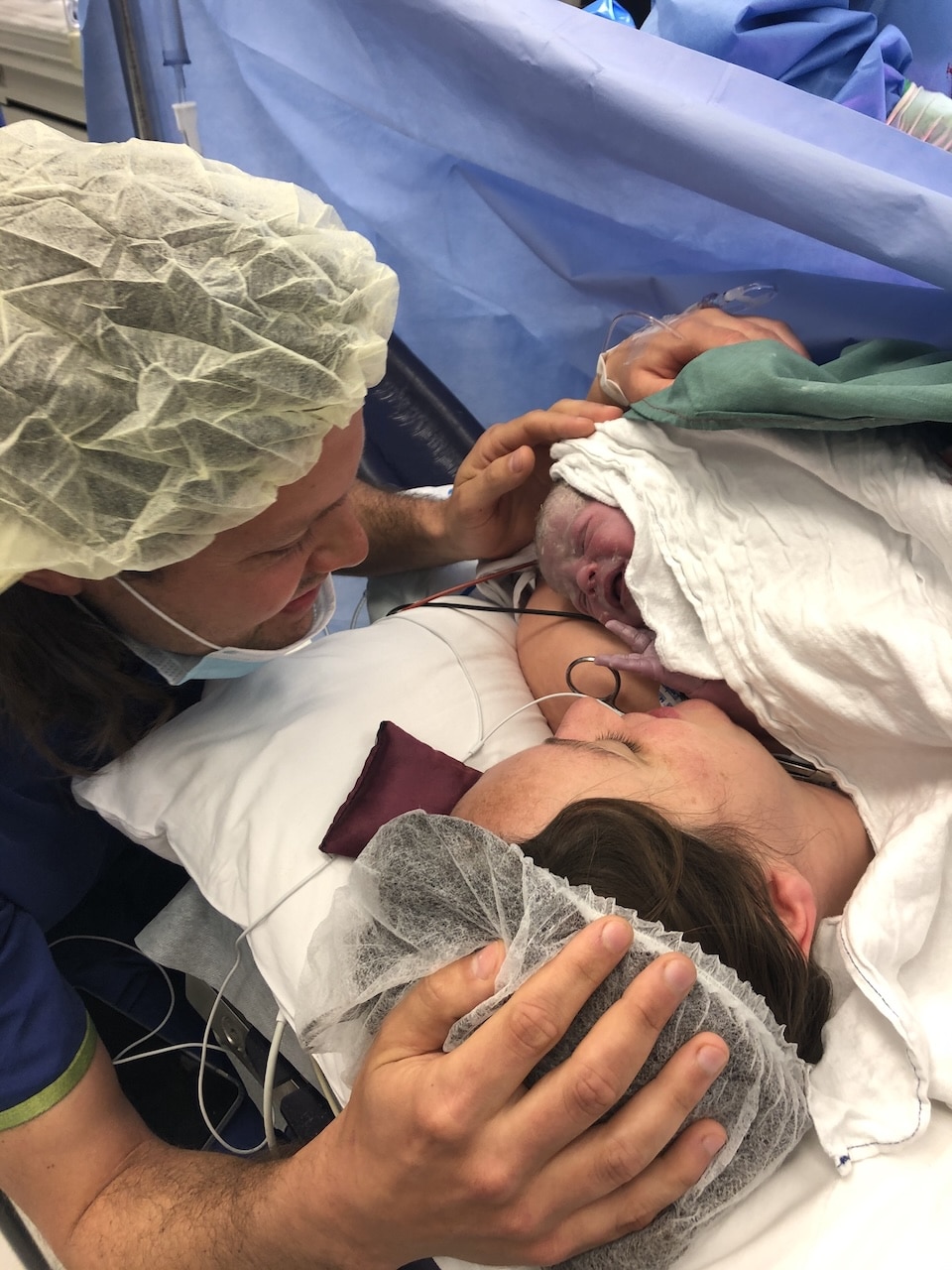
“I pushed for an hour. I could feel the contractions but Dr Bisits thought I needed a bit of help and he suggested using the forceps just till Twin A was crowning and that was an amazing option – he brought him down the birth canal and I pushed him out from there so I didn’t need an episiotomy. It was the best feeling ever to feel that relief and have him on my chest, to be the first one to hold him. He was still preterm at 35 weeks so he needed a bit of oxygen. Dr Bisits gave me an ultrasound and sure enough, within seconds twin B had turned to breech. He was quite high up and in a difficult position and no matter what we tried he wouldn’t budge. Dr Bisits told me twin B wasn’t in an ideal breech position but he’d give me one shot of birthing him aginally; he was going to do a breech extraction which involved him putting hand into my uterus and pulling him out. I felt very at peace knowing that I had a chance and if it didn’t work, I was happy to have a caesarean. But also, I was going to give it everything I could.
“Dr Bisits broke my waters, he put his arm in and I was so grateful I had the epidural because the pressure was immense. He hooked his finger around Scotty’s hip, pulled him down and I pushed from there. Scotty was little – 1.8kg – so I had a brief skin to skin and then they took him to the paediatrician and both boys went to NICU. Initially I was on top of the world – I was so euphoric – but then once I was stitched up that I didn’t have my babies.
“My recovery was so much easier which means I could be there for the twins and for Hugh. It wasn’t the postpartum I planned for but the fact that I was physically able to be present and not in pain made the process so much easier. I pumped for the first two weeks and I kept advocating for feeding them and having skin-to-skin. Sometimes it felt like they were the hospital’s baby’s not mine because I had to keep asking permission to hold them. I breastfeed them one at a time during the day and at night I tandem feed them. I also pump and give them expressed breastmilk in bottles so my husband can help. We’re also working with a lactation consultant to balance the time and also have adequate milk supply. It’s hard but we’re getting there.”




Topics Discussed
Breastfeeding, Breech Vaginal Birth, Dr Bisits, Emergency caesarean, Induction, PROM, Three babies, twin VBAC, Twins
Episode Sponsor
Today’s episode is brought to you by an Australian brand I really love, The Sleepybelly Pregnancy Pillow.
Worried about rolling onto your back during the night? Or maybe you’re tired from tossing and turning?
Experience a deeper and more restful sleep for mum and bub with Sleepybelly. The Sleepybelly is a three piece, adjustable pregnancy pillow designed to encourage safe side sleeping. Made from a super soft, air layer outer material and premium latex internally provides great support for your belly and back. Sleepybelly is Australian owned, has free shipping and comes with a 30-night trial.
Take $10 off using the Australian Birthing Stories exclusive promo code ABS10
You can purchase the Sleepybelly online today at sleepybelly.com.au
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us