Podcasts Silje
EPISODE 333
Silje

“Before I had kids I just went to the bulk billed GP but as soon as I was pregnant I wanted to find someone I connected with and I decided to do shared care with her. I didn’t want to have a specific pregnancy plan; I just took it week by week. It was a smooth, conventional pregnancy and there was nothing out of the ordinary. But towards the end I just wish I’d done more before birth preparation because by 37 weeks Mads hadn’t engaged into the pelvis and he was constantly flipping from breech to head down; they called it an unstable lie.
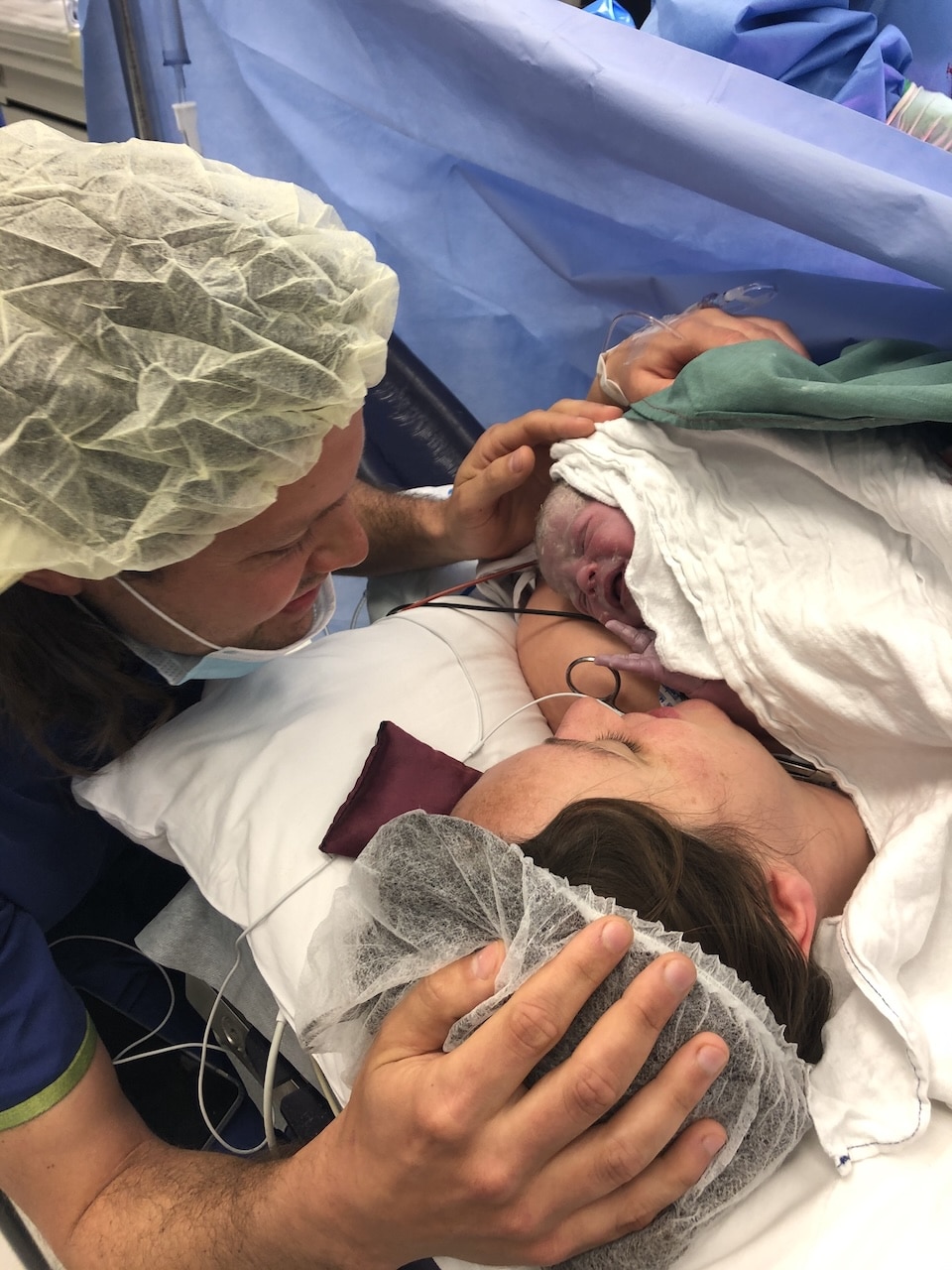
“The obstetrician offered to book me in for a planned caesarean and I agreed to that option. Jordan had to wait outside while the anaesthetist gave me the spinal block and then he came in and it all happened really quickly. I couldn’t feel the pain but there was some serious tugging and because there was a light above the operating table I could see my reflection which was quite unnerving. It all went really smoothly and they put Mads on my chest as soon as he was born and he stayed with me during recovery.”
Silje was discharged early which gave her the benefit of a home visit with a midwife. She admits it was really comforting to have the reassurance from a professional in regards to sleeping, dirty nappies and breastfeeding.
“As a first time mum I was so worried about whether he was sleeping at the right times, and I’d get frustrated if he wasn’t sleeping during the ideal nap times and I was just googling everything. With one baby I would do everything to get him back to sleep; I wish I could go back and tell myself just to let it go and move on to the next thing in the day.
“I got an IUD put in six weeks postpartum but I had to go to a gynaecologist to get it taken out. They did an ultrasound while I was there and they could tell that I had ovulated while the IUD was in which meant I was very fertile; my body had overridden the hormones. I fell pregnant on the first cycle; I had a few pregnancy tests at home and on the first one there was a very faint line. I booked in for a blood test and the GP called with the results and the hCG levels were quite low so she seemed to think I was very early in the pregnancy. I got a referral for a dating scan at 7 weeks and this was during covid – the 2021 wave that hit Sydney – and luckily I was able to bring Jordan with me because it was a standard bulk billing place. I felt so confident walking into that ultrasound and then I was absolutely thrown in the deep end.
“The sonographer went quiet and she was looking around and she asked us how we conceived. I told her we’d conceived naturally and she told me what she could see. She said there’s one over here, and there’s one over here, and there’s one over here. I told her to stop counting. At this stage she wasn’t super confident in her abilities but she said that she could see that they were all in their separate sacs with their own placentas. I knew they would have been at higher risk if they shared a sac or placenta. In a sense it was like three separate pregnancies.
“We walked out and we were just laughing at each other. I was in shock and Jordan thought it was a miracle. I was nervous, anxious, excited but I wanted to know more information as soon as possible. Jordan really calmed me and told me we’d work it out because I was thinking: could my body do it? Do we need a new car? Do we need a new house?
“I saw my GP and she was so gracious and supportive and I wanted to know how I could stay as healthy as possible. She referred me to the obstetrician at RPA because I was classed as high risk and I saw him when I was 9 weeks. I went to a twins/multiples clinic every few weeks and there was a different doctor at every appointment.
“I was so tired and my nausea and food aversions were definitely worse than my first pregnancy but I never threw up which surprised me. By the time I was 23 weeks I looked like I was full term; I got so big so quickly. It was scary thinking about how big I could get and how much my skin could stretch. I was going to the hospital every fortnight and the scans would take forever.
It’s a very surreal feeling having three babies kicking; my stomach looked completely mad as they moved. I could always feel when it was Ada kicking because she was very low in my pelvis. I just had to trust that everything was fine and I got scanned so often that I was quite reassured by that.
“It was a balance between how the babies were going and how I was coping. I had an iron infusion a couple of weeks before birth but it didn’t change my energy levels at all; I think when you’re carrying three babies it’s hard to get back to your baseline. My pelvic girdle pain was extreme. I saw my women’s health physio really early on because I knew a prevention plan was really important. The most painful thing to do was rolling over in bed. Towards the end I couldn’t walk very far and every time I was standing I felt like I needed to sit down.
“Every scan was smooth sailing which was a surprise. The babies were always growing at the predicted rates….it wasn’t until late in the pregnancy that they noticed that Ada’s growth had stalled. They weren’t really worried but they could see that she was having to work to get what she needed. I was also really anxious about Jordan getting covid because if he did he couldn’t be at the birth.
“At 34 weeks I felt like I was getting ready and they gave me a steroid shot but there wasn’t any space for planned caesareans for weeks which didn’t sit right with me so I really advocated for myself and they agreed to admit me on Thursday. I also did a NICU tour and that made me feel much more confident and comfortable about the babies’ arrival. On the Thursday morning I was admitted at 8am and they took me to a private room and the doctor came and told me that I could expect to have the babies the next day which was 34+5 weeks.
“We were so excited to meet our babies but so nervous about how it was going to unfold. I had to fast from breakfast so I was just watching movies to distract myself. At around 2pm a lactation consultant came in and she helped me express some colostrum so the babies had some ready to go. And then I was wheeled down to the operating theatre. The only request I had was to know which baby was which because we had named them already.
“Ada came out first and then Teddy and Eric. Ada was brought to my face and she needed the least amount of help whereas the boys both needed CPAP so I didn’t get to see them at the birth. The room was full of people but it was my anaesthetist who kept me calm and grounded, she was amazing. All three babies went to the High Dependency Unit (HDU) in their humidicribs and I went to recovery. I couldn’t believe I’d just given birth to three babies and I couldn’t wait to see them.
“I didn’t know what to expect but the doctors kept telling me they were doing incredibly well. Ada was 1.8kg and the boys were 2.1kg and 2.3kg. I went back to my room and even though I’d been given drugs they didn’t work; my pain was getting progressively worse and I was alone. Eventually we got on top of the pain – about six hours after birth – but that middle part is so blurry. I really needed someone to advocate for me but Jordan was with the babies and I was alone. I was wheeled down to them at about 9:30pm and it was so special. The boys were already off CPAP and they put Teddy onto my chest and then within minutes I had all three babies on my chest…it was so amazing, it was what I’d worked so hard for.
“Other triplet mums had told me to breastfeed two babies and give the third a bottle; otherwise you’re constantly breastfeeding. It was encouraging that other mums had done it. I had every intention of trying but I was also open to making sure I was prioritising my mental health.
“I was in hospital for five nights and when they told us it was time to be discharged I didn’t feel ready. They were in the NICU for 19 days and they just continued to improve each day. The doctors kept telling me how well and healthy they were. It was a strange and emotional experience being away from them at night and the lactation consultants really reiterated the importance of me pumping every three hours to establish my supply so I would set the alarm through the night to express. I could log on to the app at the hospital and see my babies while I was pumping which definitely helped.
“I remember waking up one night and touching my breast and wanting my babies to be with me and I just cried and cried. They could only be discharged once they were really well established at doing the right amount of suck feeds and there was talk of Ava going home with a tube but on the last day she pulled through.
“It was a bit of a military operation on the day of discharge. We got there for their 9am feed; two got breastfed, one got a bottle of expressed breast milk and then we put them in their pram and got out of there. My mum was home when we got there and we had three dockatots on the lounge so we put one baby in each and then Mads got home from childcare and we were ready with the camera and he said: oh no, three babies!”





Topics Discussed
breastfeeding triplets, NICU, Triplets born via caesarean section, Two planned caesareans
Episode Sponsor
Today’s episode is brought to you by Bliss Birth.
Bliss Birth is founded on the belief that women’s bodies are incredible things, and that when it’s safe, choosing natural options makes for the best outcomes for mums and babies.
That’s why Ariel has developed a range of products to support your natural birth experience. Introducing the most advanced natural pain management device for labour available in Australia – The Elle TENS Plus.
TENS stands for Transcutaneous Electrical Nerve Stimulation and it is the ultimate birth tool as it maximizes your body’s natural pain-fighting abilities.
For $89 you can hire an Elle TENS through Bliss Birth. The Bliss Birth TENS Hire features; Built-in contraction timer, Longer 8 week hire period, Pre-addressed, prepaid return (No printer needed). The ‘Mama Bag’ valued at $10.95 is yours to keep!
You can enjoy 10% off Bliss Birth with the code AUSTRALIANBIRTHSTORIES. Head over to BlissBirth.com.au
Categories
Related Products
-
Birth Meditations
$49.00Narrated by Sophie Walker, these soothing and informative meditations help you feel supported and confident around birth.
Join the conversation
Sign up to get the latest updates, freebies, podcast releases straight into your inbox
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us
@AustralianBirthStories
Follow along with us